From Duterte to Marcos: COVID stays but response changes
(Second of two parts)
MANILA, Philippines—The new administration led by President Ferdinand “Bongbong” Marcos Jr. was given six months to prepare and kickstart its COVID-19 response plan before 2022 ended.
As the Marcos administration took over, it inherited a slew of health-related problems from the previous administration, including the task of managing those beyond the administration’s control, mainly COVID.
Before Marcos, the government under then-President Rodrigo Duterte had been criticized for his pronouncements and threats against those who would refuse to comply with his pandemic policies—curfews, lockdowns, and vaccination against SARS Cov2, the virus that causes COVID.
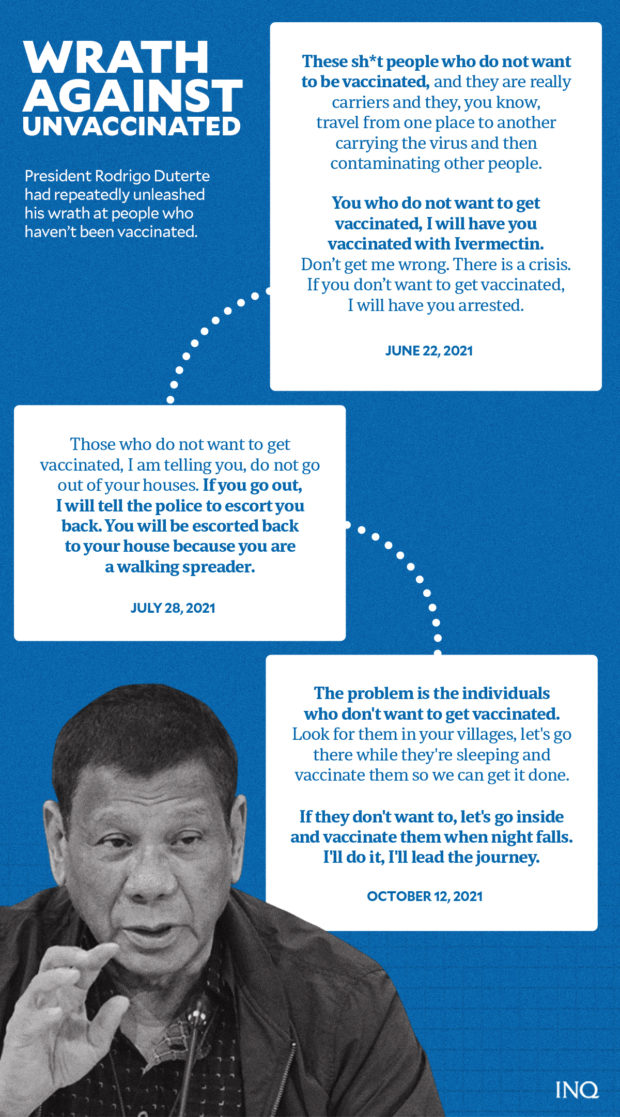
Then President Duterte’s COVID response was made controversial by some of his statements against the unvaccinated. GRAPHIC Ed Lustan
Then President Duterte’s COVID response was made controversial by some of his statements against the unvaccinated. GRAPHIC Ed Lustan
The Department of Health (DOH), particularly then-Health Secretary Francisco Duque III, also had its share of controversies during the pandemic.
In a bid to address pandemic-related issues left behind by the Duterte administration, Marcos vowed to fix the previous administration’s flaws and shortcomings in the government’s response to COVID-19.
“There were shortcomings in the COVID-19 response. We will fix them, out in the open, no more secrets in public health,” Marcos said at his inaugural speech last June 30.
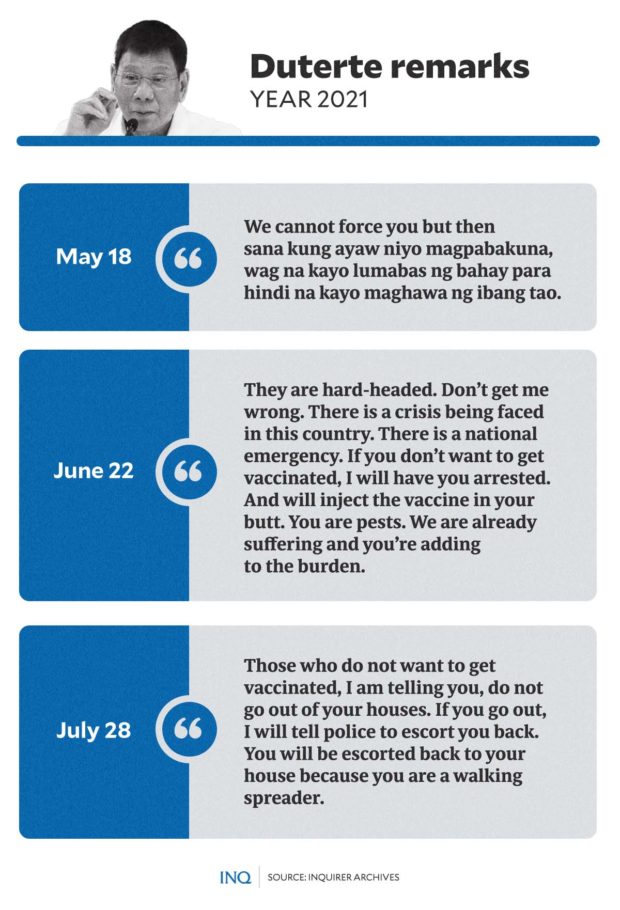
THEN President Duterte’s controversial statements were considered harmful to an efficient response to the COVID pandemic. GRAPHIC Ed Lustan
THEN President Duterte’s controversial statements were considered harmful to an efficient response to the COVID pandemic. GRAPHIC Ed Lustan
However, as the year ends, while the Marcos administration has imposed a few pandemic-related policies, it has also fallen short of addressing some key challenges and issues needed to manage COVID.
In this second part of the COVID-19 yearend report, INQUIRER.net details the hits and misses of the current administration’s pandemic management and response, the COVID-19 situation in numbers, and the vaccination progress in the country.
The report will also cite a health expert and his assessment of the Marcos administration’s COVID response, his thoughts on long COVID and endemicity, and his projection on the country’s COVID-19 cases.
Mask mandate: An economic decision
Aside from keeping his promise not to impose lockdowns in the country this year, Marcos has issued an executive order allowing the voluntary wearing of face masks indoors and outdoors—despite threats and cases of emerging COVID-19 variants and sub-variants.
Last October, Marcos signed Executive Order (EO) No. 7, allowing the optional use of face masks in indoor and outdoor settings, except in health care facilities, medical transport vehicles, and public transportation.
However, the elderly, persons with comorbidity, immunocompromised individuals, pregnant women, unvaccinated individuals, and symptomatic persons are still being encouraged to wear face masks.
READ: It’s official: Wearing masks indoors, outdoors now voluntary
An earlier version of the policy, EO No. 3, which allowed the optional wearing of face masks in outdoor settings, was repealed.

ONE of the biggest controversies that hounded the COVID response of the Duterte administration were revelations that billions of pesos had been transferred to Pharmally, then a newly-formed company that bagged huge contracts. GRAPHIC Ed Lustan
ONE of the biggest controversies that hounded the COVID response of the Duterte administration were revelations that billions of pesos had been transferred to Pharmally, then a newly-formed company that bagged huge contracts. GRAPHIC Ed Lustan
The orders were issued despite objections and concerns from the medical community and other experts—most of whom cited the country’s positivity rate, which has yet to slide down, as well as the unattained booster target, saying that it is “not yet time” or “too early” to lift the face mask rule.
READ: Mask outdoors now optional: Taking risks vs COVID
According to health reform advocate and former special adviser to the National Task Force on COVID-19 Dr. Tony Leachon, Marcos’ decision to ease the use of face masks in the country is an “economic decision.”
“[T]he President, on a periodic basis, consults the business sector,” Leachon told INQUIRER.net, adding that “based on several reports,” Marcos seeks advice from the health cluster of the Private Sector Advisory Council (PSAC).
The PSAC, composed of business leaders and experts from various industries, seeks to aid the government in achieving its economic objectives.
READ: Sabin Aboitiz named as Private Sector Advisory Council head
“That’s why you can learn from the decision of the President on the relaxation of the restrictions including the masking—[that] this is, more or less, an economic and business decision rather than a medical thing,” Leachon said.
Had Marcos consulted a medical expert, according to Leachon, the expert might support the decision to open businesses without restrictions and lockdowns as long as it is anchored on maintaining the Minimum Public Health Standards (MPHS)—“with the wearing of the face masks as the guide post”—and if the government is stepping up its booster campaign.
READ: To wear, or not wear, face masks vs COVID: The zigzag road PH is taking
“In the event that we don’t have a very high booster rate, I think the President should have maintained the mask mandate, knowing that sub-variants—with the opening of borders—will come to our shores, considering these would come from other countries,” Leachon added.
By the numbers: COVID in PH
Data from the DOH showed that as of December 13, the country’s COVID-19 caseload had reached 4,056,239—with 17,900 tagged as active cases, 3,973,275 as recovered, and 65,064 died.
Among the regions with the highest COVID-19 cases were:
- National Capital Region (NCR): 1,305,651
- CALABARZON (Cavite, Laguna, Rizal , Quezon): 725,031
- Central Luzon: 399,415
- Western Visayas: 216,964
- Central Visayas: 208,850
The provinces and cities with the most cases in the country were:
- Quezon City: 274,212
- Cavite: 241,852
- Laguna: 181,085
- City of Manila: 164,317
- Rizal: 157,794
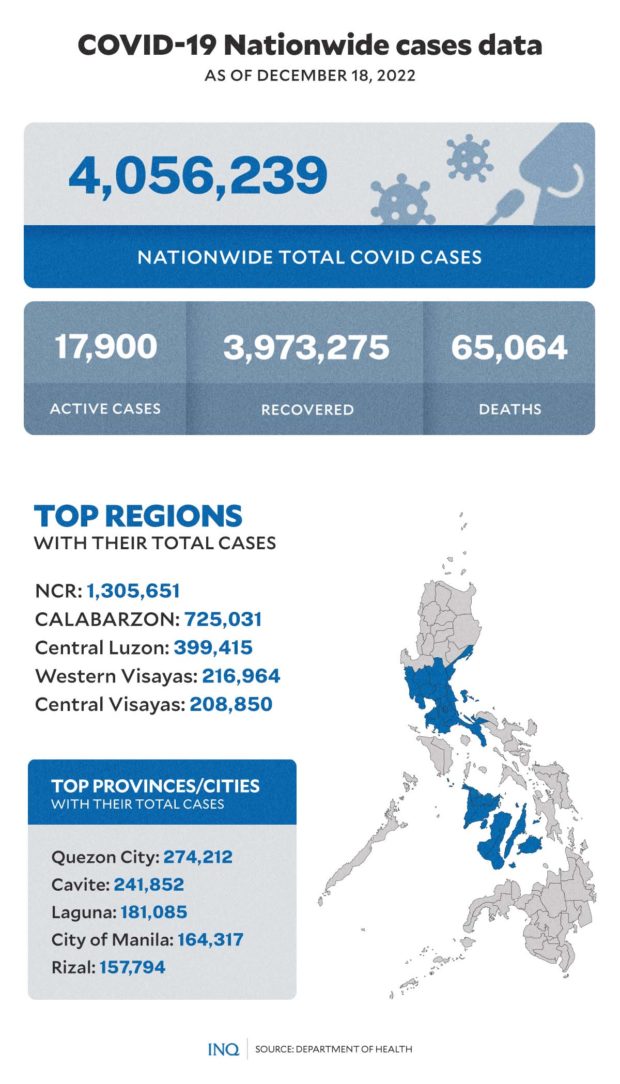
THE COVID-19 nationwide cases data as of December 18 based on data from the Department of Health. GRAPHIC Ed Lustan
THE COVID-19 nationwide cases data as of December 18 based on data from the Department of Health. GRAPHIC Ed Lustan
The biosurveillance report based on sequence results released last November 21 to 24 showed that among the COVID-19 variants and sub-variants present in the Philippines include:
- XBC variant: 532 cases
- Omicron BA 2.3.20: 3,485 cases
- Omicron BA.2.75: 35 cases
- Omicron BA.4: 324 cases
- Omicron BA.5: 12,559 cases
- Omicron BQ.1 (a BA.5 sub-lineage): 16 cases
- Omicron XBB: 684 cases
The University of the Philippines-Philippine Genome Center (UP-PGC) Main, Visayas, and Mindanao, Research Institute for Tropical Medicine (RITM), San Lazaro Hospital (SLH), and Southern Philippines Medical Center (SPMC) also noted the increase in the number and proportion of the BA.5 sub-lineage of Omicron since July 2022.
They also stated that the BA.2.3.20 and XBB sub-variants “have been on a continuous uptrend starting September 2022.”
The nationwide positivity rate as of December 4 was 12.3 percent, far exceeding the World Health Organization’s (WHO) moderate (5 percent or below positivity rate) and low (2 percent or below positivity rate) classifications.
Citing November 30 data, OCTA Research fellow Guido David on December 2 noted that Metro Manila’s COVID-19 positivity rate also increased from 9.4 percent on November 23 to 11.9 percent.
“This rate of increase in the positivity rate in the NCR is around the same rate of increase during the Omicron BA.5 wave (from June) and the XBB (from September). This projects to a December BQ.1 wave similar to the top BE.5 and XBB waves,” David pointed out in a Twitter post.
READ: Metro Manila’s weekly new COVID-19 cases up 56% — OCTA
The positivity rate, however, will only be used for “internal monitoring” as the health department shifts its focus on COVID-19 response from keeping virus transmission low to “reducing vulnerability.”
The DOH will mainly use three metrics to determine the alert levels of areas: total bed utilization rate, average daily attack rate, and vaccination coverage. Other metrics—case growth rate, severe and critical admissions, deaths, and positivity rate—will only be used for “internal monitoring.”
Alethea De Guzman, DOH Epidemiology Bureau director, said the positivity rate is no longer a “proper measure of the actual COVID-19 situation.”
READ: DOH shifts focus in COVID-19 response
However, David disagreed with the DOH’s decision, saying that “[t]he positivity rate, being a percentage, is more reliable than ADAR (average daily attack rate), which is underestimated because of low testing and affected by backlog.”
"the positivity rate is no longer a proper measure of the actual COVID-19 situation."
I disagree. The positivity rate, being a percentage, is more reliable than ADAR, which is underestimated because of low testing and affected by backlog.
Read more: https://t.co/3nbYkmaid5— Dr. Guido David (@iamguidodavid) December 1, 2022
Vaccination progress, wastage
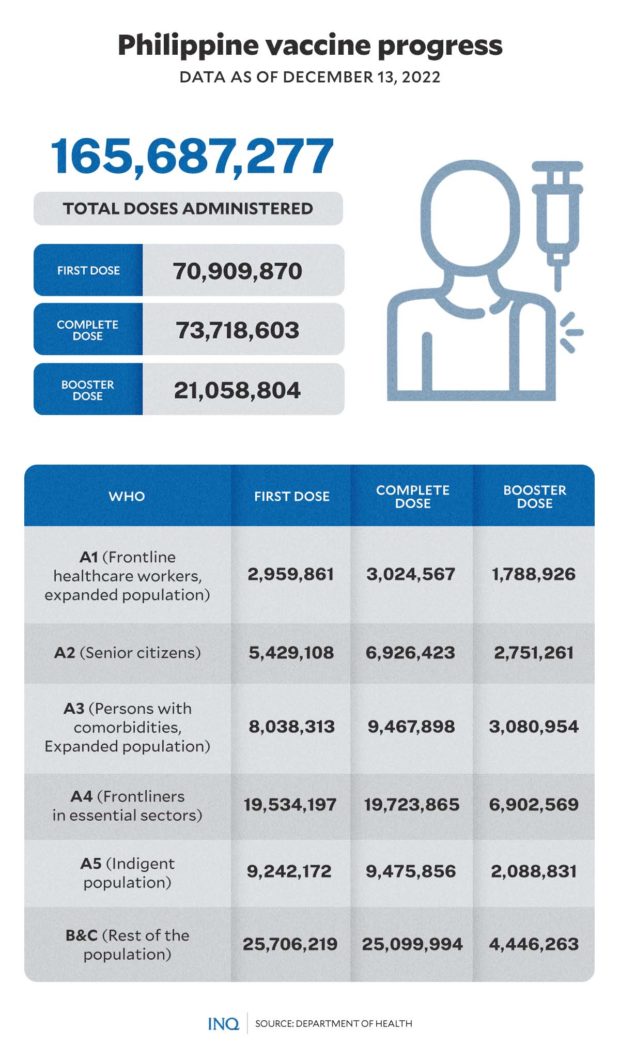
According to data from the National COVID-19 Vaccination Dashboard, 70,909,870 individuals had already received their first dose of the COVID vaccine as of December 13.
At least 73,718,603 people were already fully vaccinated during the same period, which covers 94.39 percent of the government’s target to vaccinate 70 percent of the total population—or around 78,100,578.
At least 6,926,423 senior citizens, or individuals under the A2 priority group, were able to receive a full dose of vaccines, which is at least 79.42 percent of the target to vaccinate 85 percent of the elderly population in the country.
At least 21,058,804 individuals had already been inoculated with a booster dose against COVID-19.
Last April, the government started giving second COVID-19 booster doses for selected priority groups to increase protection against COVID and its versions.
As of November, second boosters are still only available for three priority groups: healthcare workers, the elderly, and individuals with comorbidity aged 18 and up.
The health department has yet to expand coverage for the second booster doses to the rest of the population despite rising COVID-19 vaccine wastage rate in the country, which Vergeire pegged at 17.5 percent or 44 million vaccine doses—above the WHO’s threshold of vaccine wastage at 10 percent.
READ: No ramping up 2nd booster coverage despite dose wastage
Vergeire noted that 75 percent of the vaccine wastage came from the procurement of private sector and local government units, while 24 million doses expired.
At least 3.8 million doses have been affected by “operational wastage” due to “natural disasters, temperature excursions, and discoloration.”
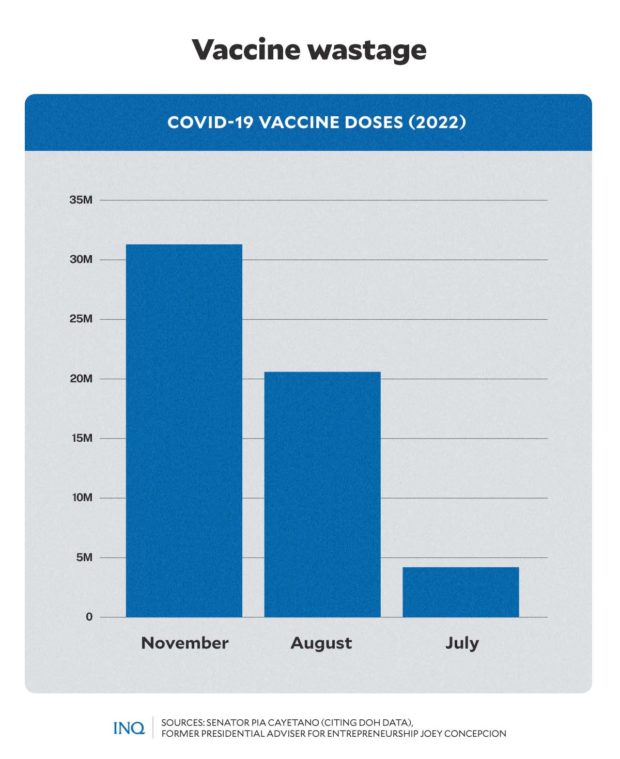
DATA released by several senators revealed COVID-19 vaccine wastage amid emerging variants and sub-variants of SARS-SoV-2 in the country. GRAPHIC Ed Lustan
DATA released by several senators revealed COVID-19 vaccine wastage amid emerging variants and sub-variants of SARS-SoV-2 in the country. GRAPHIC Ed Lustan
The DOH said negotiations with bivalent vaccine developers Moderna and Pfizer were still ongoing, with health authorities set to go through different clearances for regulation.
READ: Gov’t checking out bivalent COVID-19 vaccines
READ: What to know about ‘bivalent vaccines’ that target Omicron
Marcos Jr’s score
When asked what score he would give the Marcos administration for its COVID-19 pandemic response this year, Leachon said he would give it a seven out of ten or 70 percent—higher than the 60 percent score he gave the Duterte administration.
“The [pandemic response during] Duterte administration, with due respect with them, had alleged anomaly,” Leachon explained, citing controversial deals between the DOH and Pharmally Pharmaceuticals Corp. for overpriced PPE and other COVID items investigated by the Senate last year and the wastage of P31.3 million worth of vaccines.
“[I gave] 70 percent for the Marcos administration because it has not been a full year yet. However, it already had problems such as the lack of a secretary of health, even though his main problem is health,” Leachon explained.
In a recent statement, Marcos said he still has no nominee yet for the top DOH post and added that DOH OIC Undersecretary Maria Rosario Vergeire is “doing a fine job.”
“We have not yet nominated someone for DOH Secretary,” Marcos said.
The President earlier said that he would name a health secretary once the country’s coronavirus situation “normalizes” from its current state of calamity.
READ: Gov’t told: Permanent DOH chief needed now, not later
Leachon also cited the voluntary mask mandate under the current administration as one of his reasons for the score he gave.
“[The mandatory wearing] of face masks, which is our protection while the booster rate remains low, was removed. It’s counter-intuitive to remove the main support to prevent people from getting infected—all while the country still doesn’t have its secretary of health and the government is not upgrading its booster plan,” he said.
“What I can see is that while there’s no alleged corruption, the administration has a lack of vision and sense of urgency, which is important in this particular time,” he added.
“We need a quick economic recovery backed with an excellent health plan. Having a good health plan can accelerate the country’s economic recovery.”
Endemicity?
Last month, the DOH advised experts to be very careful when using the term endemic.
“We need a thorough evaluation by experts. It takes time. It takes about three to five years because we need to monitor if it will stabilize and if there will be low transmission in an area before we can say a disease is endemic. We do not just use this term. We need a basis,” said Vergeire.
“Endemic is a technical term, it is an epidemiologic term, and I advise people who are talking to the media to be very careful when they speak of these things because when the public hears this, they may be complacent,” she added.
READ: DOH counters OCTA: ‘Thorough evaluation’ needed to declare an endemic
The term endemic came from the Greek word éndēm(os). Its prefix en- means “in or within,” and combined with the Greek root “demos” or people, the term’s basic meaning is “within a certain people” or “within a certain area.”
Endemic, as defined by Dictionary.com, means “natural to, native to, confined to, or widespread within a place or population of people.” It is also most commonly used to describe a disease prevalent in or restricted to a particular location, region, or population.
The Mailman School of Public Health described endemic as “a disease outbreak that is consistently present but limited to a particular region. This makes the disease spread and rates predictable.”
Some endemic diseases, which are still common to date, include influenza, malaria, HIV, measles, tuberculosis, and cholera.
An endemic disease, according to WHO, is constantly present in a population within a particular region. The endemicity of a disease, according to WHO, is based on a disease’s rate of spread.
READ: COVID as endemic disease: Not weaker but forever with us
Throughout the year, despite the emergence of new COVID variants and sub-variants, several experts mentioned about COVID-19 being endemic in the country.
Last November 15, infectious disease expert Dr. Edsel Salvana—also a member of the DOH Technical Advisory Group—claimed that COVID-19 is heading to the endemic phase in the Philippines.
“What we are seeing here with COVID, it seems that it is becoming endemic in the sense that it will circulate like a cold. It will not disappear completely,” Salvana said in a televised briefing.
However, the DOH reiterated that it remains uncertain if COVID-19 will soon be endemic in the country.
“We can say, yes, endemicity will come soon. But now, it’s quite uncertain because of the [low] immunity we are talking about,” Vergeire said.
READ: DOH uncertain if COVID-19 nearing endemicity
Leachon echoed the DOH’s views, saying that the country has yet to reach endemicity.
“We cannot say that we are in the endemic phase since there are still emerging COVID variants. The WHO has also not yet declared that COVID-19 is no longer a Public Health Emergency of International Concern, meaning we’re still in a pandemic,” he said.
“I don’t think we have to declare victory too soon, with due respect to my very good friend Dr. Salvana, I don’t think we are in the endemic stage.”
He added that statements claiming that the country has reached the endemic phase could “confuse the public” and influence some people’s attitude toward vaccination.
“If you get out that kind of message, no one will be willing to vaccinate, and people would also stop wearing face masks. We will send the wrong signal that we’re okay when actually we’re not yet okay,” Leachon said.
What lies ahead?
According to Leachon, cases of COVID-19 in the country might increase before the year ends amid the emerging variants and sub-variants.
“I think it will increase because we are no longer taking enough RT-PCR tests, and we are not checking enough,” he said.
“However, even though cases might increase, these will be mild cases that can be treated at home, isolated, and augmented by antiviral drugs. I expect that the infections will rise due to increased mobility during the holiday season, but we are much ready right now, and we are in a better position than last year, so we will be fine,” he added.
TSB
For more news about the novel coronavirus click here.
What you need to know about Coronavirus.
For more information on COVID-19, call the DOH Hotline: (02) 86517800 local 1149/1150.
The Inquirer Foundation supports our healthcare frontliners and is still accepting cash donations to be deposited at Banco de Oro (BDO) current account #007960018860 or donate through PayMaya using this link.