Fighting for breath: Pneumonia continues to kill children worldwide
MANILA, Philippines—As the fight to reduce deaths from pneumonia continues, numbers show that infection of the lungs remains one of the biggest killers of children worldwide.
Pneumonia, as defined by the World Health Organization (WHO), is a kind of acute respiratory infection that hits the lungs. When a person has pneumonia, the alveoli—the tiny air sacs in the lungs—are filled with pus and fluid, “which makes breathing painful and limits oxygen intake.”
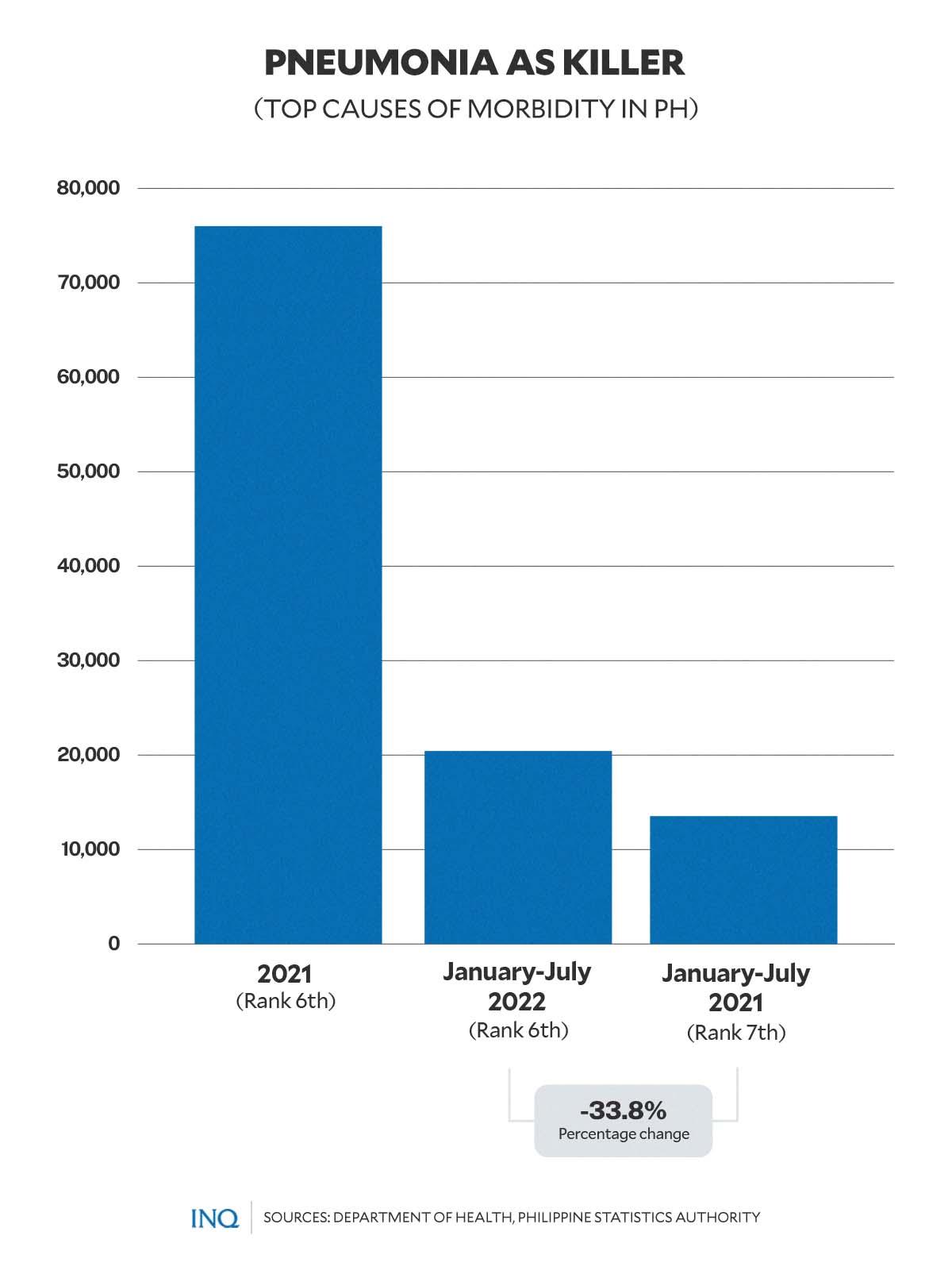
In the Philippines, pneumonia remains to be among the top causes of death.
Based on preliminary data from the Philippine Statistics Authority (PSA), as of August 2022, pneumonia ranked sixth as the top 10 causes of mortality in the country, causing the deaths of 13,536 people.
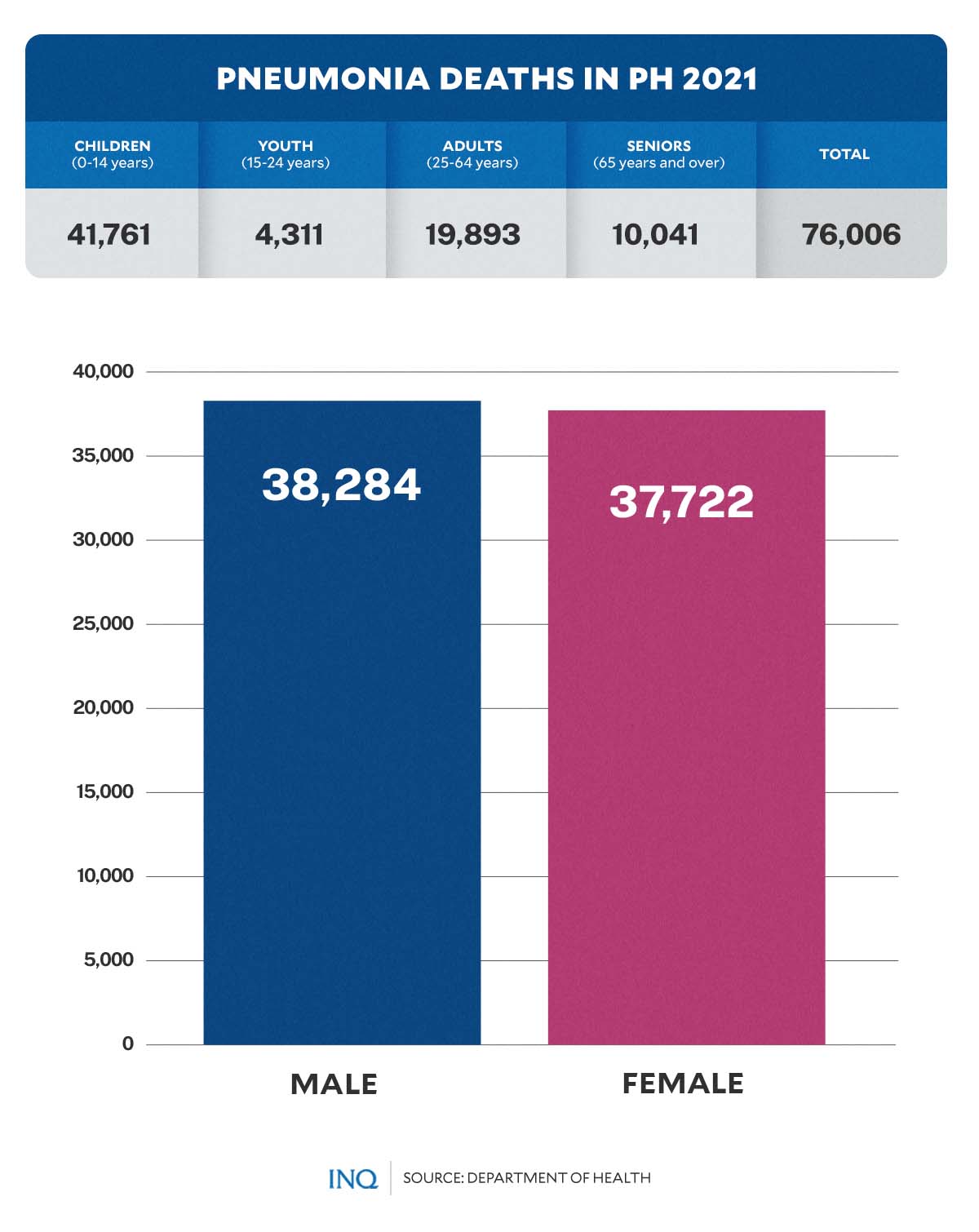
Last year, figures from the 2021 Field Health Services Information System (FHSIS) report by the Department of Health (DOH) showed that pneumonia killed over 76,000 people in the Philippines.
Article continues after this advertisementAlarmingly, the data also presented high mortality among Filipino children—a portion of a larger data that show how deadly pneumonia is among children across the globe.
Article continues after this advertisementPneumonia in children
There are over 1,400 cases of pneumonia per 100,000 children worldwide, or one case per 71 children every year. Data from Unicef showed that the greatest incidence occurs in South Asia (2,500 cases per 100,000 children) and West and Central Africa (1,620 cases per 100,000 children).
Worryingly, Unicef emphasized that a child dies of pneumonia every 43 seconds.
In 2019, pneumonia killed over 740,000 children younger than 5 years old globally, accounting for 14 percent of all deaths of children under the age of 5, but 22 percent of all deaths in children aged 1 to 5 years.
According to the US Centers for Disease Control and Prevention (CDC), the figure was “greater than the number of deaths from any infectious diseases, such as HIV infection, malaria, or tuberculosis.”
While pneumonia affects children and families across the globe, WHO stressed that deaths are highest in southern Asia and sub-Saharan Africa.
In the Philippines, a total of 41,761 children under the age of 15 died from pneumonia last year. These deaths, based on the 2021 FHSIS report, include:
- 256 deaths among newborn babies and 6-day-old infants
- 520 deaths among 7 to 28-day-old infants
- 10,515 deaths among babies aged 29 days to 11 months
- 20,104 deaths among children aged 1 to 4 years
- 7,378 deaths among 5 to 9-year-old children
- 2,988 deaths among children aged 10 to 14 years.
An article published in the Pediatric Infectious Disease Society of the Philippines (PIDSP) Journal noted that “in Filipino children below 5 years of age, [pneumonia] is the most common cause of death, accounting for about 14% of all causes of mortality.”
However, all these cases and deaths are preventable.
Simple solutions save children’s lives
Cases and deaths due to pneumonia among children can be prevented through simple interventions, according to WHO. The infection can also be treated with “low-cost, low-tech medication and care.”
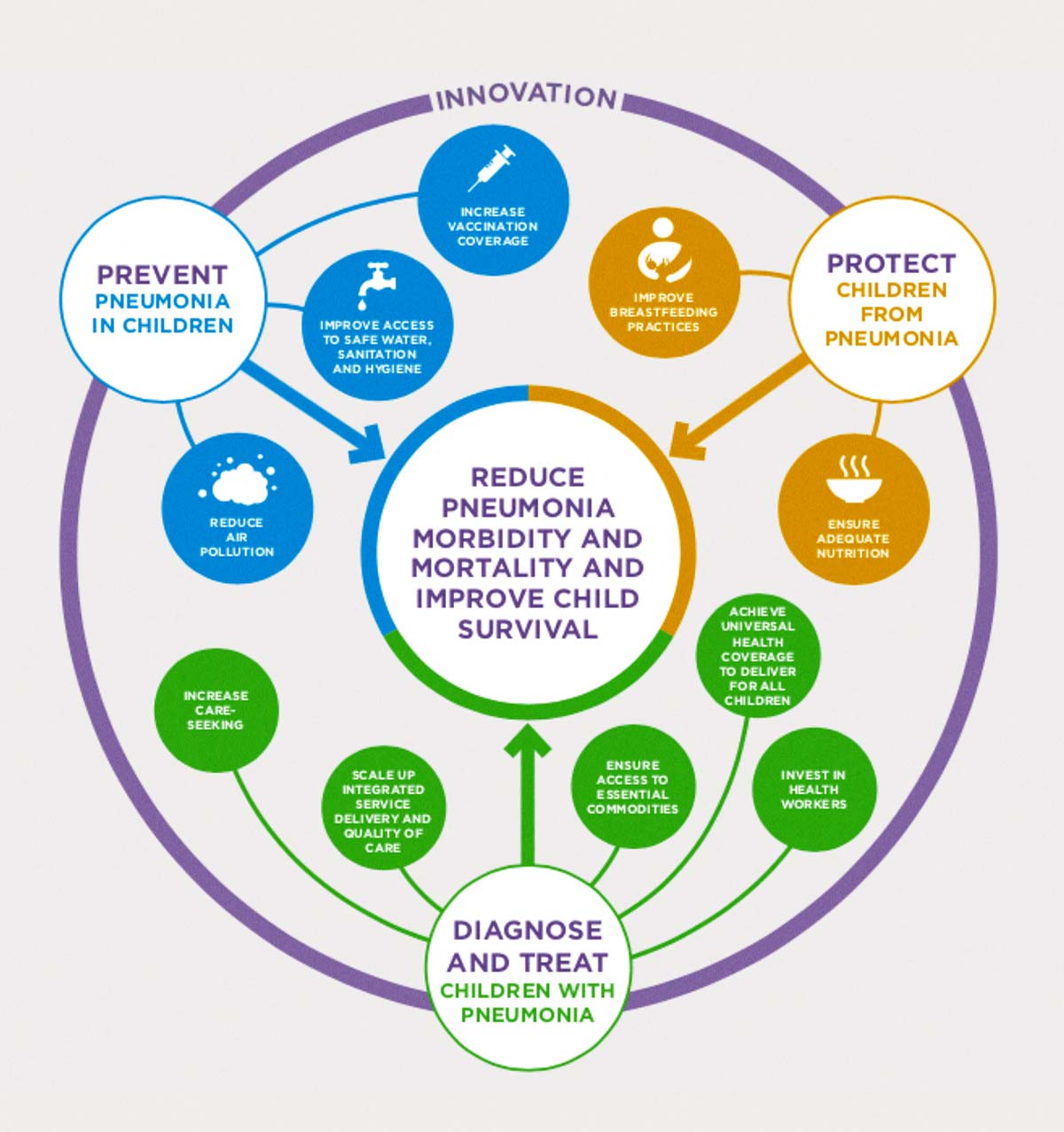
In 2013, WHO and Unicef launched the Integrated Global Action Plan for the Prevention and Control of Pneumonia and Diarrhea (GAPPD), an integrated framework of key interventions proven to effectively protect children’s health, prevent diseases, and treat children who experience diarrhea and symptoms of pneumonia.
The GAPDD follows the “protect, prevent, and treat” framework.
Protect—“Protective interventions provide the foundations for keeping children healthy and free of disease,” including:
- Exclusive breastfeeding (without additional food or liquids, including water) for the first six months of an infant’s life to protect them against diseases and guarantee a food source that is safe, clean, accessible, and perfectly tailored to their needs.
- Provide children good nutrition through complementary feeding—providing children with adequate quantities of safe, nutritious, and age-appropriate foods alongside continued breastfeeding—to help strengthen their strong immune systems, protect them from diseases, and reduce child deaths, including those due to pneumonia and diarrhea.
Prevent—Preventive interventions to help stop disease transmission and prevent children from becoming infected
- Immunization: Haemophilus influenzae type b (Hib) and pneumococcal conjugate vaccines (PCV) are effective in preventing pneumonia. Vaccines against measles and pertussis in national immunization programs substantially reduce acute respiratory infections (ARI), including pneumonia, and death in children.
- Reduced household air pollution: Improved household air quality can reduce cases of severe ARI.
- HIV prevention: Preventing HIV and treating HIV infections can help maintain the immune system and reduce the risk of contracting ARI.
Diagnose and treat—Urgent action and recognizing the danger signs of ARI (including fast and difficult breathing and coughing) is the first step in saving children against diseases such as pneumonia, according to WHO and Unicef.
Antibiotics is the usual treatment for most types of serious ARI, which typically cost less than 50 cents. However, WHO and Unicef cautioned that not all children with ARI symptoms must be given antibiotics.
“According to the WHO and UNICEF Integrated Management of Childhood Illness guidelines, only those cases classified by a health worker as pneumonia or severe ARI should be treated with antibiotics. Moreover, not all children classified as such have true ARI,” the organizations said.
“That said, in settings without adequate diagnostic tools, the WHO/Unicef guidelines provide a common standard by which health workers can assess and classify bacterial ARIs requiring antibiotic treatment.”
Economic burden
However, not all children with ARI can get treatment.
Data from Unicef showed that poor children living in rural areas are less likely to get treatment for symptoms of pneumonia than their wealthier and urban peers.
Only less than two-thirds—or about 60 percent—of children with symptoms of ARI globally were taken to a healthcare provider in 2021.
“Although it cannot be assumed that all children with symptoms have bacterial ARI and should receive antibiotics, the data indicate a big gap in the likelihood of treatment between the richest and the poorest (72 percent and 55 percent, respectively),” Unicef said.
Around 57 percent of children with symptoms of ARI who are living in rural areas were taken to a health facility, while 64 percent of their peers from urban areas were given medical attention.
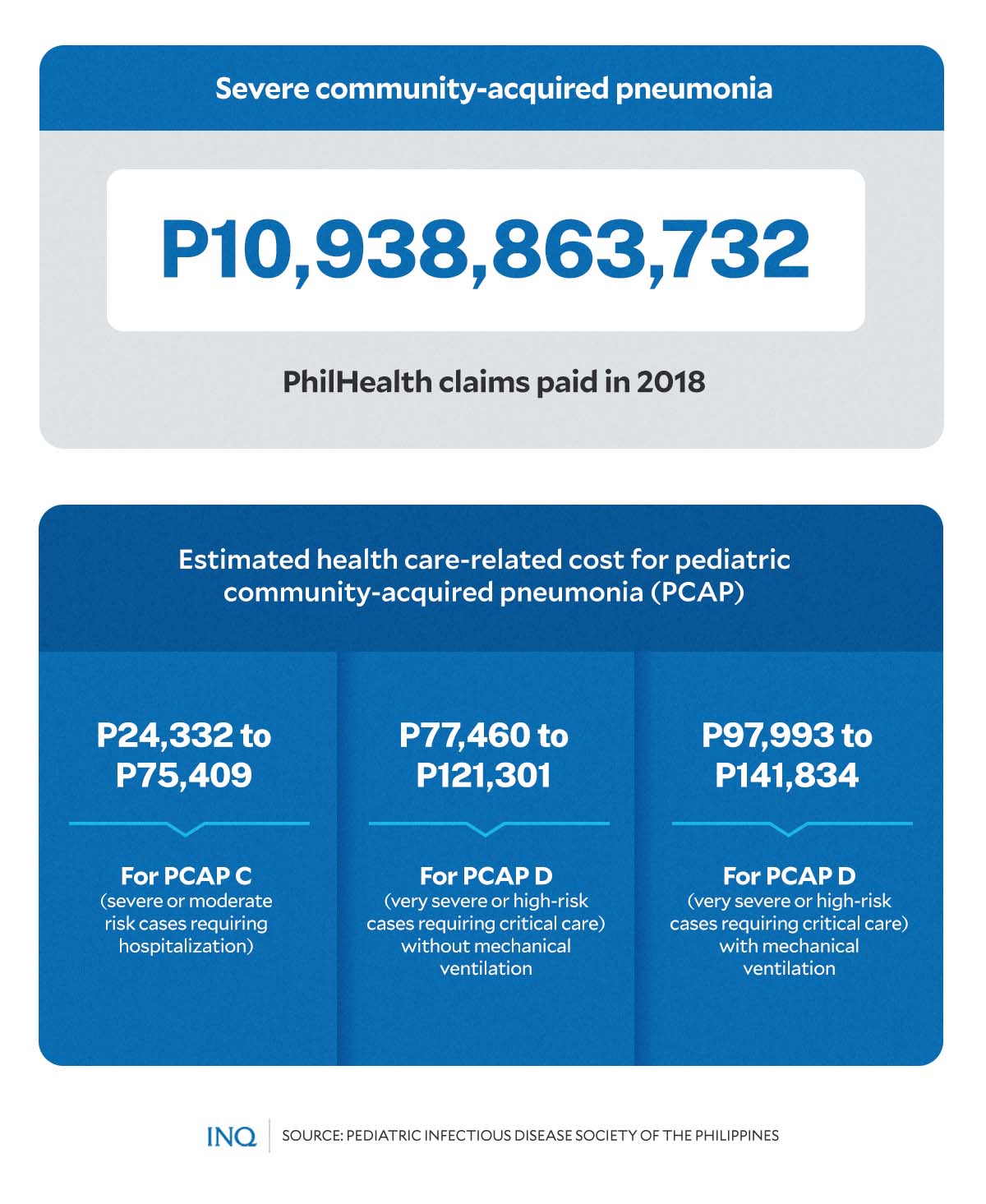
Dr. Jaime A. Santos, former head of the Infectious Disease Section of the Philippine Children’s Medical Center, said in his article in the PIDSP Journal that the economic burden of pneumonia in the Philippines is huge.
Citing data from the Philippine Health Insurance Corporation (PhilHealth), among claims processed by PhilHealth in 2018, community-acquired pneumonia (CAP) ranked number one—with a total of P10,938,863,732 worth of claims processed for severe CAP (CAP III).
Citing another study, Santos noted that the estimated healthcare-related cost for pediatric CAP (PCAP) amounted to:
- P24,332 to P75,409: for PCAP C (severe or moderate risk cases requiring hospitalization)
- P77,460 to P121,301: for PCAP D (very severe or high-risk cases requiring critical care) without mechanical ventilation
- P97,993 to P141,834: for PCAP D (very severe or high-risk cases requiring critical care) with mechanical ventilation.
“The estimated health care cost of hospitalization is markedly higher than the PhilHealth case rate payments. As per the study results, the economic burden of pneumonia is, thus, significantly higher than PhilHealth estimates,” the authors of the study concluded.
RELATED STORIES:
Pediatric vaccination hesitancy by parents: Science provides answers
COVID worsens ‘largest backslide’ in child vaccinations in 30 years