The mystery of anosmia, loss of smell, and its COVID links
MANILA, Philippines—Over two years into the pandemic, scientists are now beginning to uncover more about how SARS-CoV-2—the virus behind the disease COVID-19—causes loss of smell, as well as some possible treatments to address the condition.
Anosmia, or the partial or complete loss of sense of smell, has since been considered one of the telltale signs of COVID-19.
According to Dr. Charles Greer—professor of neurosurgery and neuroscience, vice chair for research, and director of interdepartmental neuroscience graduate program at Yale School of Medicine—around 30 percent of COVID-19 patients experience anosmia.
“The public reports describe anosmia before the onset of other symptoms as well as afterwards, with patients regaining their sense of smell very quickly after recovery,” said Greer in an article published by the Yale Medicine Magazine.
A year ago, little was known about COVID-19. The connection between the disease and loss of smell among COVID-19 patients was also unexplained—making anosmia a “mysterious” symptom of the disease.
Article continues after this advertisementHowever, recent studies are finally making progress in yielding answers as to how SARS-CoV-2 leads to loss of smell in some patients. Multiple potential treatments for anosmia were also undergoing clinical trials.
Article continues after this advertisementScience behind COVID-19 and loss of smell
A study in 2020, early in the pandemic, showed that the SARS-CoV-2 virus attacks and damages cells in the nose called the sustentacular cells which, according to an article published in Nature Journal, provide nutrients and support to odor-sensing neurons.
A few years later, a newer study uncovered some clues about how the SARS-CoV-2 virus impacts the olfactory neurons—which help detect and transmit odorant information to the central nervous system—and what happens after an infection.
In the study, biochemist Stavros Lomvardas and his co-researchers at Columbia University in New York City found that people who had died from COVID-19 “had fewer membrane-embedded receptors for detecting odor molecules than usual” even though their neurons were still intact.
Researchers explained that the olfactory neuron’s nuclei—whose chromosomes are organized into two compartments—had been “scrambled.”
According to researchers, the chromosomes in the olfactory neuron’s nuclei are normally organized into two compartments. This type of structure, a Nature article wrote, “enables the neurons to express specific order receptors at high levels.”
Lomvardas and his co-researchers, after looking at the autopsied neurons of some people who had died from COVID-19, said “the nuclear architecture was unrecognizable.”
Some studies found that structural changes in the brain of some people infected by COVID, including tissue damage in areas linked to the brain’s olfactory center.
Other studies have also pointed out that a certain genetic mutation might cause some people to become more susceptible to loss of smell or taste.
Condition dwindles under new variants
A study published in 2020 reviewed 32 papers on the reported prevalence of loss of smell, taste, or both among a combined sample of 20,451 COVID-19 patients.
Researchers found that the estimated global pool prevalence among 19,242 COVID-19 patients from the 27 sample studies was 48.47 percent.
Meanwhile, loss of taste was reported in 20 studies and 8,001 patients with an estimated pool prevalence of 41.47 percent, while 13 studies reported a combined loss of smell and taste among COVID-19 patients with an estimated pool prevalence of 35.04 percent.
READ: Systematic Review and Meta-analysis of Smell and Taste Disorders in COVID-19
A slightly similar study was conducted among COVID-19 patients admitted at the Quezon City General Hospital (QCGH) between July and September 2020.
The patients, who participated in the study, were asked to answer an offline version of the American Academy of Otolaryngology-Head and Neck Surgery AAO-HNS COVID-19 Anosmia Reporting Tool prior to undergoing COVID-19 RT-PCR testing.
The study found that 36.6 percent—63 out of 172 COVID-19 patients—experienced anosmia or loss of smell. Around 65 percent—41 out of 172—reported anosmia as the first COVID-19-related symptom they had.
“A significantly higher proportion of patients with anosmia were positive for COVID-19 than those without anosmia at 95.2% and 52.3% respectively. The risk for COVID-19 among patients with anosmia was almost two times higher than those without anosmia,” the researchers noted.
READ: Association of Anosmia and Positive SARS-CoV-2 (COVID-19) RT-PCR Test Results Among Patients in the Quezon City General Hospital
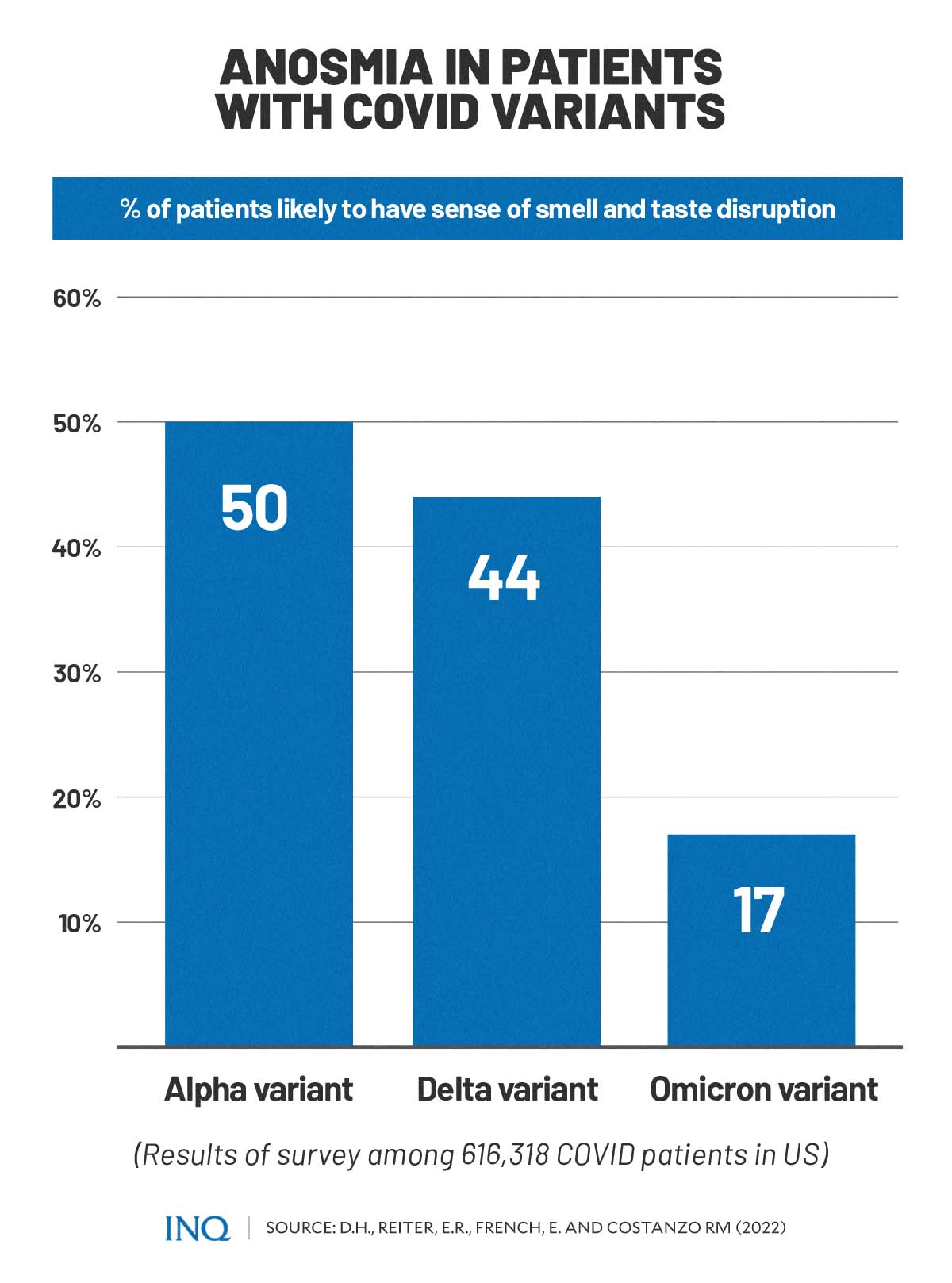
A recent study in the United States, however, showed that anosmia among COVID-19 patients is starting to become less common as the SARS-CoV-2 virus mutates to different variants.
The study, which surveyed 616,318 people who have had COVID-19, found that those who have been infected with the Alpha variant—the first variant of concern—were only 50 percent likely to have chemosensory disruption or issues in sense of smell and taste.
Researchers also discovered that the probability of experiencing loss of smell or taste fell to 44 percent for patients who contracted the later Delta variant and 17 percent for the Omicron variant.
READ: Decreasing Incidence of Chemosensory Changes by COVID-19 Variant
READ: Among now Greek letter-named COVID variants, Delta draws biggest fear
READ: Omicron: What science knows so far about latest Greek-lettered COVID variant
READ: The uncertainty of treating Omicron as sign of pandemic end game
Long-term smell loss
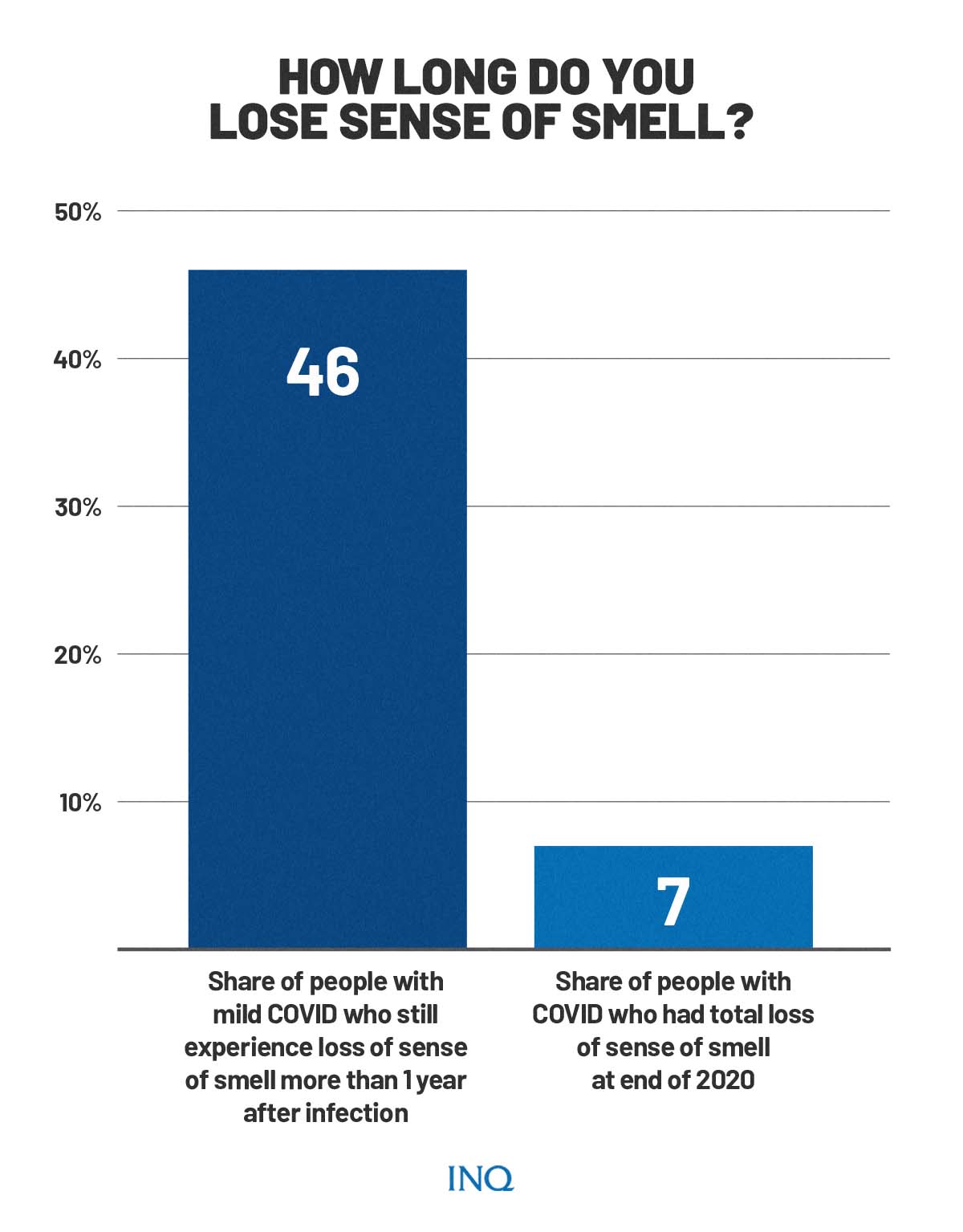
A separate study last year, however, saw that a significant portion of people who got COVID-19 early in the pandemic still experience loss of smell, taste, or both.
Out of the 100 people observed for the study, 46 percent still have issues with their sense of smell more than a year after contracting COVID-19. There was also 7 percent who still had a total loss of smell by end of 2020.
“Given that more than 500 million cases of COVID-19 have been confirmed worldwide, tens of millions of people probably have lingering smell problems,” an article in Nature Journal noted.
According to United Kingdom’s National Health Service (NHS), loss of or change in sense of smell or taste could be a possible long COVID-19 symptom.
“It can take time for your sense of smell or taste to recover. You may find that foods smell or taste differently after having coronavirus,” the NHS said.
“These changes don’t usually last long, but they can affect your appetite and how much you eat. For a very small number of people, your change of sense of smell or taste may be more long-term,” it added.
World Health Organization (WHO) and the US Center for Disease Control and Prevention (CDC) said symptoms may last for more than four weeks and they can come and go or relapse over time, while symptoms of long COVID can persist from the initial illness or appear after recovery.
READ: Understanding ‘long COVID’ and how to prevent it
Earlier this year, Health Undersecretary Leopoldo Vega warned that 10 percent to 15 percent of COVID-19 patients in the Philippines may possibly experience long COVID.
READ: ‘Long COVID’ possible in 10- 15% of infected persons — DOH
Finding answers and treatments
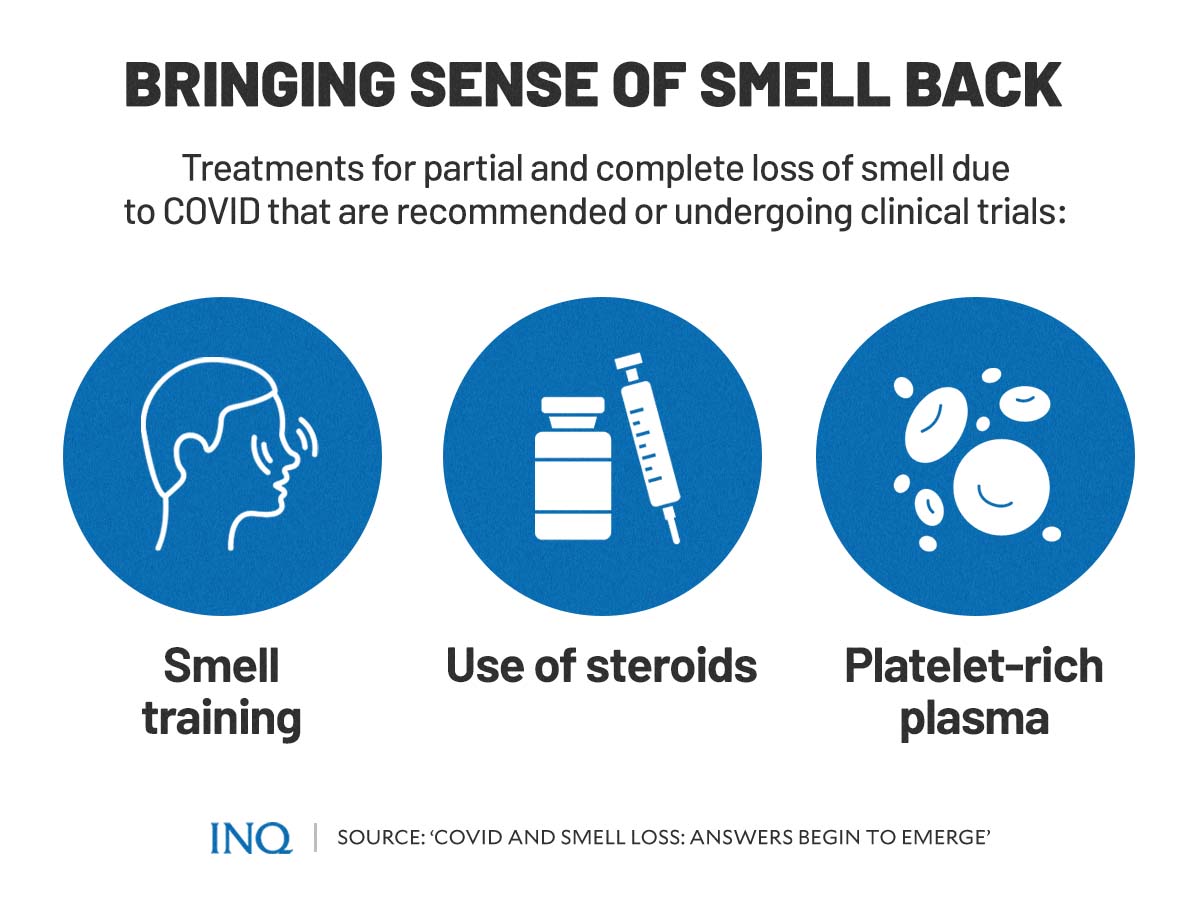
As researchers uncover more information about the connection between SARS-CoV-2 and loss of smell, many treatments are also undergoing small clinical trials at the same time.
However, many of these treatments for anosmia due to COVID-19 are still in their early days of testing. For now, studies point out a recommended possible solution for the phenomenon: smell training.
According to Danielle Reed, a geneticist at the Monell Chemical Senses Center in Philadelphia, Pennsylvania, patients undergoing smell training are given samples of strong-smelling substances.
The treatment’s aim is for the patients to sniff and identify the substances. This, hopefully, will lead to the restoration of olfactory signaling.
However, Reed said the method might work only with people who have partial smell loss after getting infected with COVID-19.
Other possible treatment options based on ongoing studies include using steroids to reduce inflammation—inflammation, studies found, plays a part in smell disruption—or through platelet-rich plasma made from patients’ own blood.
READ: Your own blood can heal you
“The reality is that the study will take the rest of this year to run, and it’ll take us probably to the middle of next year before we analyse the data and report it,” said Carl Philpott, a nose and sinus specialist at the University of East Anglia in Norwich, UK.
“If we find a positive benefit, our next job will be to apply for more funding to do a full stage trial.”
TSB
For more news about the novel coronavirus click here.
What you need to know about Coronavirus.
For more information on COVID-19, call the DOH Hotline: (02) 86517800 local 1149/1150.
The Inquirer Foundation supports our healthcare frontliners and is still accepting cash donations to be deposited at Banco de Oro (BDO) current account #007960018860 or donate through PayMaya using this link.