Understanding ‘long COVID’ and how to prevent it
MANILA, Philippines—Amid warnings about the possible uptick of COVID-19 cases in the country paired with the possible entry of more transmissible Omicron sub-variants, experts in the Philippines—and across the globe—are urging governments to focus also on cases of long COVID.
At a Laging Handa briefing last week, Dr. Ted Herbosa, an adviser to the National Task Force against COVID-19, said that medical professionals “are starting to see cases of long COVID” in the Philippines.
“We are monitoring and recording it. We will also register it and we will count and study it so that we will know the situation of long COVID in the Philippines,” he said.
READ: Gov’t now also focusing on ‘long COVID’ cases
Some studies conducted in other countries have also shown cases of long COVID in over a million individuals who have previously been infected with SARS-CoV-2, the virus that causes COVID-19.
In this article, INQUIRER.net will provide more details about long COVID including its symptoms, who are at most risk of experiencing it, the efficacy of vaccines in preventing long-term COVID impacts, and how people can protect themselves against it.
‘Long COVID’
Most people who contracted COVID-19 fully recover within weeks or months. However, recent studies and data found that some people who have been infected with the SARS-CoV-2 virus can experience “a variety of mid-and long-term effects after they recover from their initial illness.”
These mid-and long-term effects, according to World Health Organization (WHO), are collectively known as post-COVID-19 condition or long COVID.
“Post COVID-19 condition, also known as ‘long COVID,’ refers collectively to the constellation of long-term symptoms that some people experience after they have had COVID-19,” said WHO.
The condition is also called long COVID, long-haul COVID, post-acute COVID-19, post-acute sequel of SARS CoV-2 infection (PASC), long-term effects of COVID, and chronic COVID by others.
Meanwhile, people who experience it refer to themselves as “long-haulers.”
“Post COVID-19 condition is defined as the illness that occurs in people who have a history of probable or confirmed SARS-CoV-2 infection; usually within three months from the onset of COVID-19, with symptoms and effects that last for at least two months,” WHO explained.
“The symptoms and effects of post-COVID-19 condition cannot be explained by an alternative diagnosis. Post COVID-19 condition can affect a person’s ability to perform daily activities such as work or household chores,” it added.
It is still unclear what exactly causes long COVID.
According to Johns Hopkins Medicine, it could be due to organ damage, a persistent inflammatory or autoimmune response, or other reasons.
Since there is not enough data yet on long COVID, health experts said it is still difficult to predict how long the post-COVID-19 condition will last for a patient.
“There is much to learn about the post-COVID-19 condition, but current research shows that patients can experience lingering symptoms for weeks to months following COVID-19. The research also shows that patients can improve with time,” WHO said.
The United States Centers for Disease Control and Prevention (CDC), meanwhile, said that long COVID can last for weeks, months, or even years.
Three types
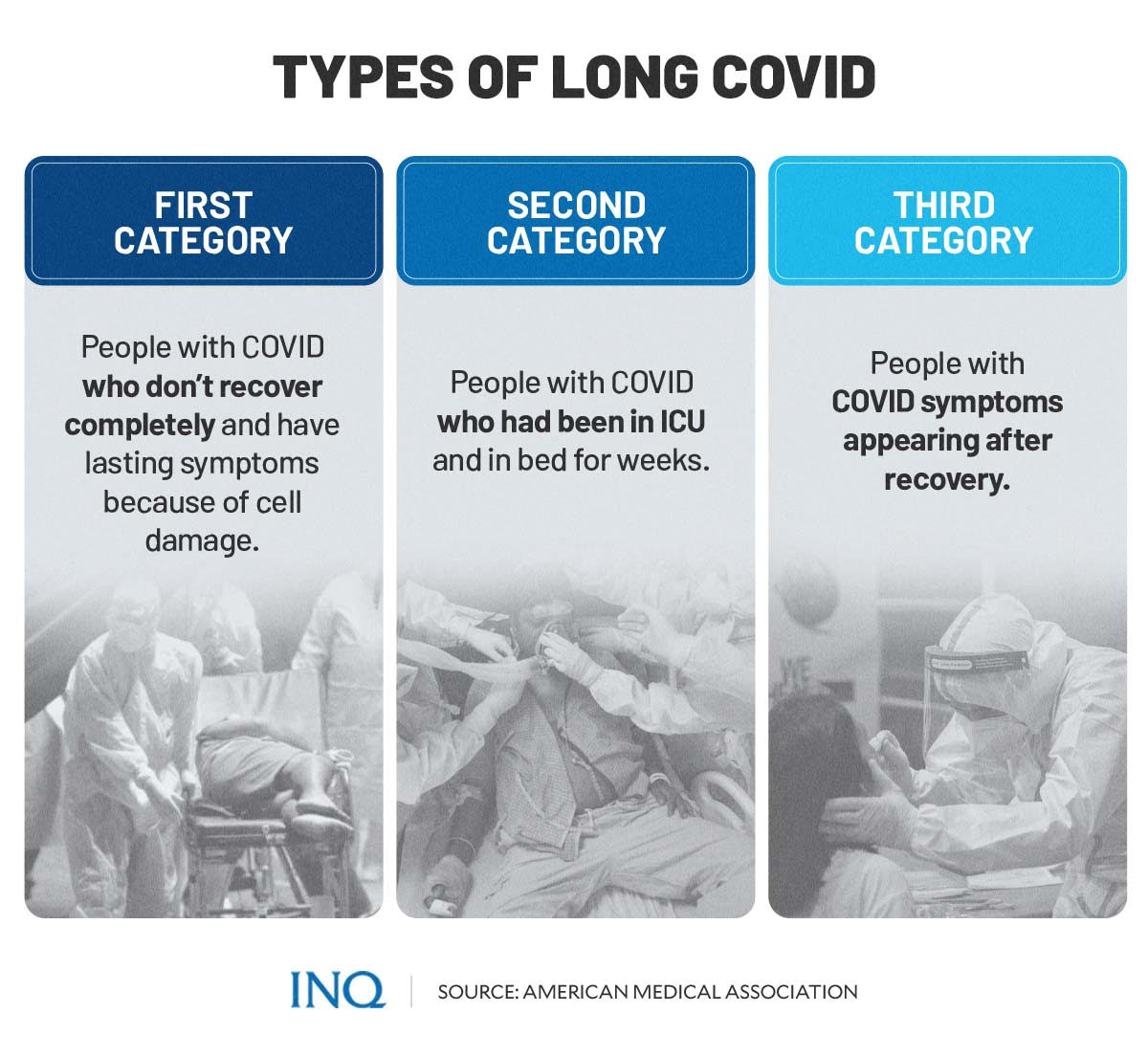
In an article on the American Medical Association’s (AMA) website titled “What doctors wish patients knew about long COVID,” AMA member Dr. Devang Sanghavi said that there are three types or categories of long COVID.
READ: What doctors wish patients knew about long COVID
The first category, according to Sanghavi, involves people with COVID-19 who “do not recover completely and have ongoing symptoms because of direct cell damage from the virus.”
“COVID-19 itself has direct cell damage because of the virus and this can cause lingering symptoms,” Sanghavi said in the article.
The next category of long COVID involves people whose “symptoms are related to chronic hospitalization.” This includes patients in the intensive care unit (ICU) of hospitals who are in bed for weeks.
“There is inherent muscle weakness. There is inherent cognitive brain dysfunction. There is inherent psychosocial stress-causing post-traumatic stress disorder-like syndrome, which we call post-ICU care syndrome,” Sanghavi explained.
The third category was characterized as cases in which symptoms occur or appear after recovery from COVID-19.
What are the symptoms?
Long COVID, according to WHO, is usually diagnosed three months after COVID-19.
“This allows the health care provider to rule out the normal recovery process after illness,” said WHO.
The symptoms of long COVID can persist from the initial illness or appear after recovery. Both WHO and US CDC said symptoms may last for more than four weeks and they can come and go or relapse over time.
“Post-COVID conditions may not affect everyone the same way. People with post-COVID conditions may experience health problems from different types and combinations of symptoms happening over different lengths of time. Most patients’ symptoms slowly improve with time,” the US CDC said.
“However, for some people, post-COVID conditions may last months, and potentially years, after COVID-19 illness and may sometimes result in disability,” it added.
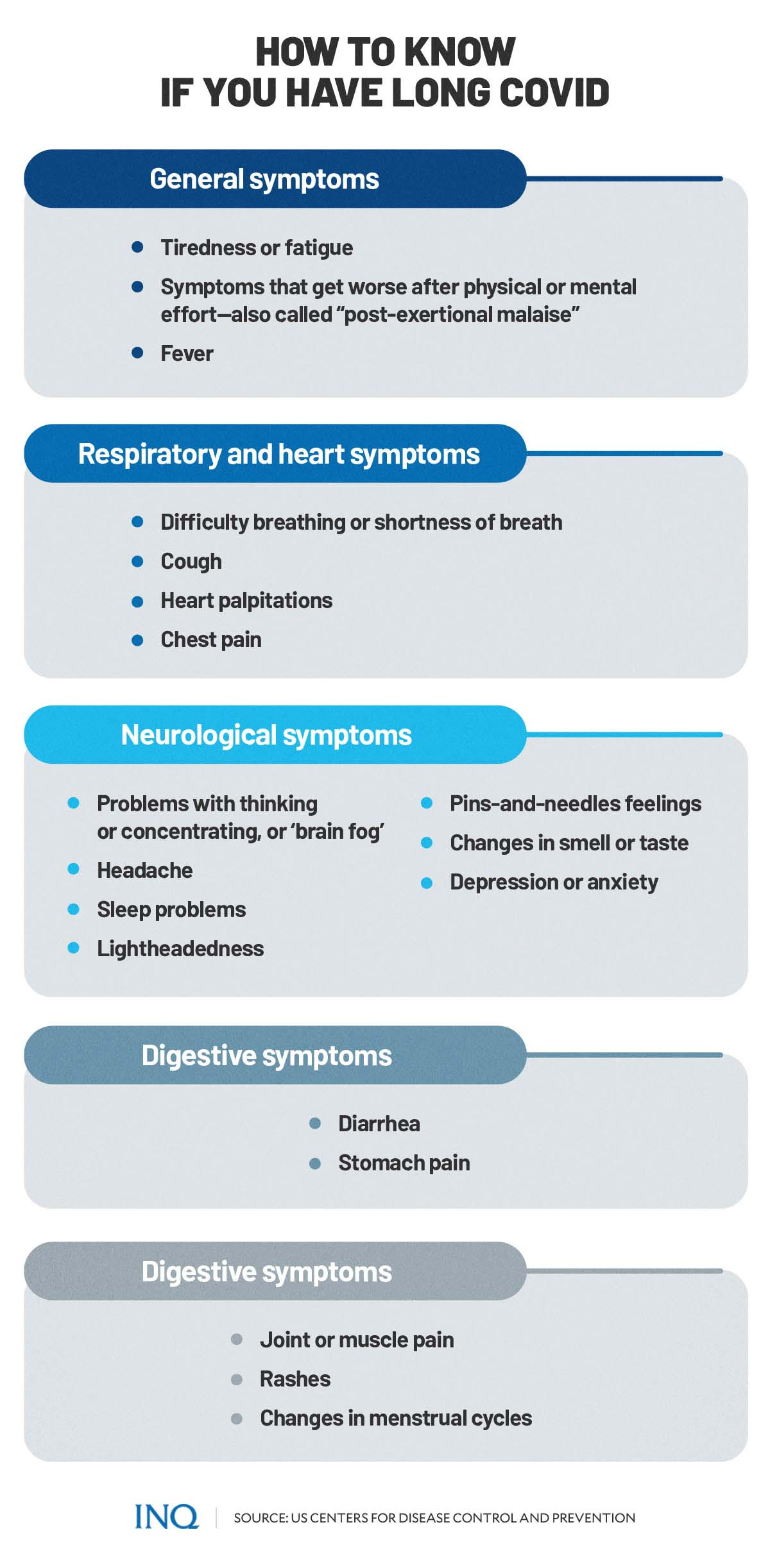
Some of the commonly reported symptoms of long COVID include:
General symptoms:
- Tiredness or fatigue
- Symptoms that get worse after physical or mental effort—also called “post-exertional malaise”
- Fever
Respiratory and heart symptoms:
- Difficulty breathing or shortness of breath
- Cough
- Heart palpitations or fast beating of the heart
- Chest pain
Neurological symptoms
- Having problems in thinking or concentrating—also referred to as “brain fog”
- Headache
- Sleep problems
- Lightheadedness
- Pins-and-needles feelings
- Changes in smell or taste
- Depression or anxiety
Digestive symptoms
- Diarrhea
- Stomach pain
Other symptoms:
- Joint or muscle pain
- Rashes
- Changes in menstrual cycles
The US CDC also noted that some long haulers may also develop symptoms that are difficult to explain and manage. Due to this complication, long haulers with unexplained symptoms “may be misunderstood by their health care providers” which can delay diagnosis and treatment.
Long COVID numbers
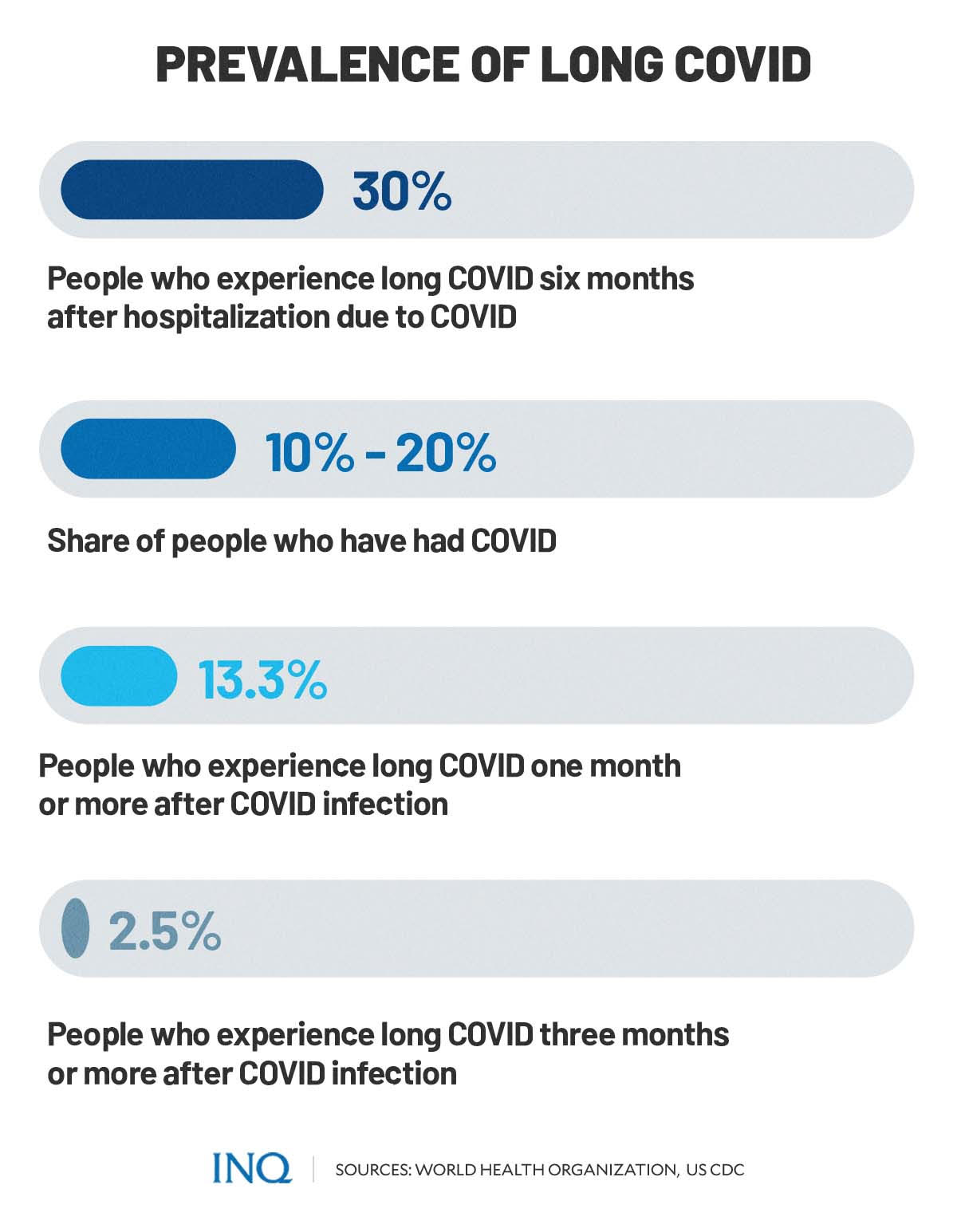
According to WHO, current evidence suggests that at least 10 percent to 20 percent of people experience long COVID.
The US CDC stated that the estimated number of people who had COVID-19 and later on experienced long COVID conditions can vary. Their data showed that:
- 13.3 percent experience long COVID at one month or longer after infection
- 2.5 percent at three months or longer (based on self-reporting)
- Over 30 percent at six months among patients who were hospitalized due to COVID-19.
In June 2021, the REACT-2 study, led by Imperial College London, found that over 2 million people in England were suspected to have had long COVID and experienced one or more COVID-19-related symptoms which lasted for at least 12 weeks.
READ: Over 2 million in England may have had long COVID, study finds
In February, research conducted in Thailand found that up to a million individuals in the country might be suffering from long COVID. This, according to the study, could lead to labor shortages in the future.
READ: Long COVID may have hit 1 million people in Thailand, survey shows
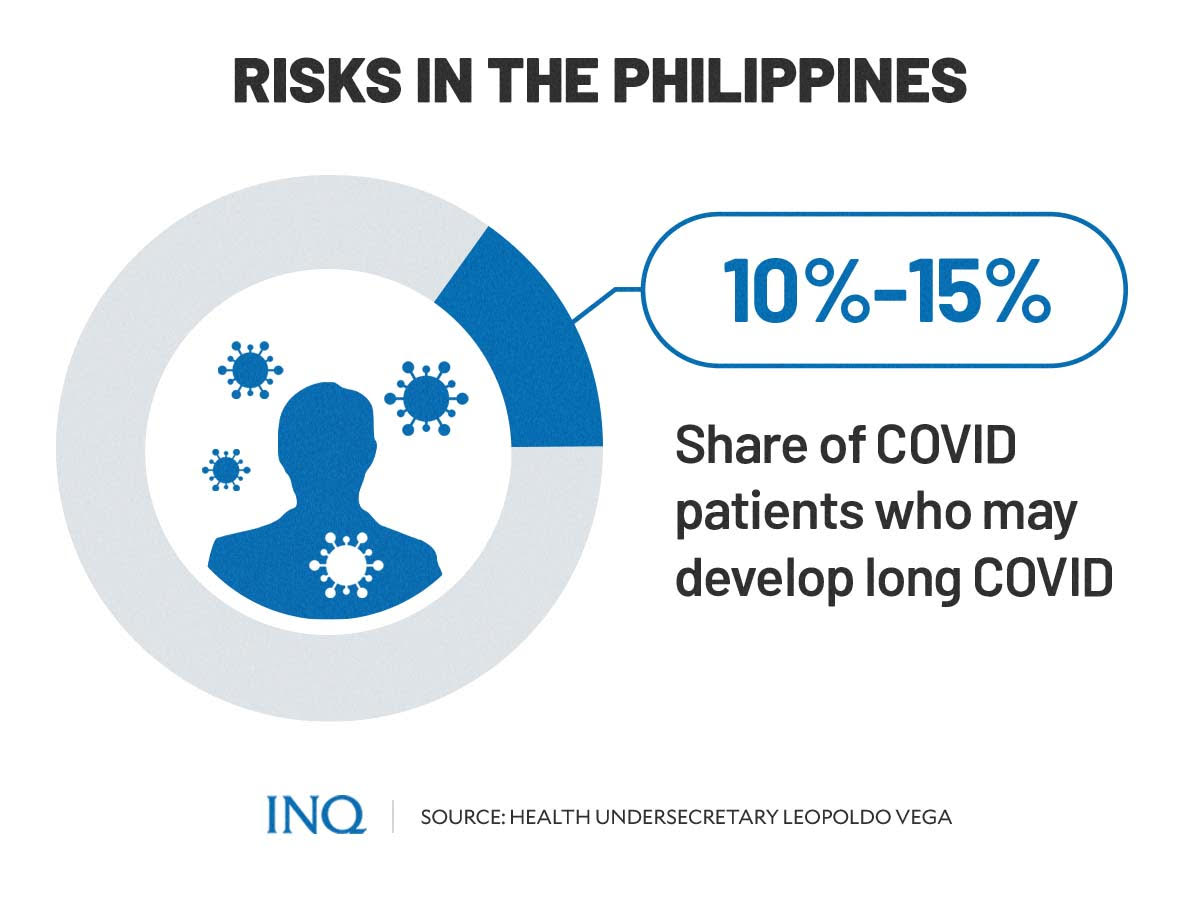
In the Philippines, Health Undersecretary Leopoldo Vega warned earlier this year that 10 percent to 15 percent of COVID-19 patients may possibly experience long COVID.
Vega explained that if a person who recently recovered from COVID-19 continues to experience health issues after 30 days, chances are he or she has long COVID.
READ: ‘Long COVID’ possible in 10- 15% of infected persons — DOH
Who is at risk?
Anyone who has had COVID-19 can develop long COVID and experience prolonged symptoms, according to WHO.
Current evidence also showed that there is no relationship between the initial severity of COVID-19 infection and the likelihood of developing long COVID condition.
The US CDC listed some examples of groups of people who are likely to be affected more by long COVID conditions based on studies. The list includes:
- People who have experienced more severe COVID-19 illness, especially those who were hospitalized or needed intensive care.
- People who had underlying health conditions prior to COVID-19.
- People who did not get a COVID-19 vaccine.
- People who experience multi-system inflammatory syndrome (MIS) during or after COVID-19 illness.
- People affected by health inequities including people from racial or ethnic minority groups and people with disabilities.
“These are examples and not a comprehensive list of people or groups who might be more at risk than other groups for developing post-COVID conditions,” the US CDC noted.
WHO advises people who think they may have developed long COVID condition or symptoms of long COVID to consult and seek care from their health care provider.
“They will help you to determine whether this is the case, and to provide you with the care you need to manage your symptoms.”
In a statement released on May 22, the Philippines’ Department of Health (DOH) also advised Filipinos to consult a doctor or health care provider if they experience prolonged COVID-19 symptoms or symptoms related to long COVID.
“To date, there is no test to diagnose long COVID,” the DOH said.
“If you experience the following, immediately go to the nearest emergency room: difficulty breathing (catching breath, can only say one word); severe chest pain; lightheadedness or fainting,” the health department added.
Can vaccines reduce risk of long COVID?
While available vaccines were proven to help protect people against COVID-19, a recent study found that vaccines may provide less protection against long COVID condition.
Based on a study of more than 13 million, researchers found that the COVID-19 vaccine reduces the risk of long COVID among individuals by only about 15 percent.
“We’re literally solely reliant, now almost exclusively, on the vaccine to protect us and to protect the public,” said nephrologist Ziyad Al-Aly, who was among the authors of the study published in Nature Medicine—a monthly peer-reviewed medical journal.
“Now we’re saying it’s only going to protect you 15%. You remain vulnerable, and extraordinarily so,” Al-Aly added.
READ: Long COVID after breakthrough SARS-CoV-2 infection
Long COVID care and protection
One thing about long COVID is that it cannot be passed on to others.
On the other hand, there is no specific medication therapy yet for people with long COVID condition. WHO said data suggesting holistic care, including rehabilitation, can be helpful.
“Breathing exercises, physical therapy, medications, and other treatments can help improve your health, but be prepared for a gradual recovery,” Johns Hopkins Medicine suggested.
Despite the low protection provided by vaccines against long COVID—based on recent studies—and the lack of available treatments for the condition, WHO said people can still protect themselves against long COVID.
One way to do it is to avoid getting infected with the SARS-CoV-2 virus.
“This includes getting vaccinated and following the many public health and social measures that can reduce your chances of getting infected and spreading the COVID-19 virus,” WHO said.
“The best way to protect yourself against COVID-19 is to do a combination of actions, and as WHO commonly says ‘Do it all!’.”
These include:
- Keeping physical distance of at least 1 meter from others
- Wearing a well-fitted mask over your nose and mouth at all times
- Opening windows
- Coughing or sneezing into your elbow
- Cleaning your hands frequently
- Getting vaccinated as soon as it is your turn
TSB
For more news about the novel coronavirus click here.
What you need to know about Coronavirus.
For more information on COVID-19, call the DOH Hotline: (02) 86517800 local 1149/1150.
The Inquirer Foundation supports our healthcare frontliners and is still accepting cash donations to be deposited at Banco de Oro (BDO) current account #007960018860 or donate through PayMaya using this link.