Mpox: What is it, how it spreads, care for patients
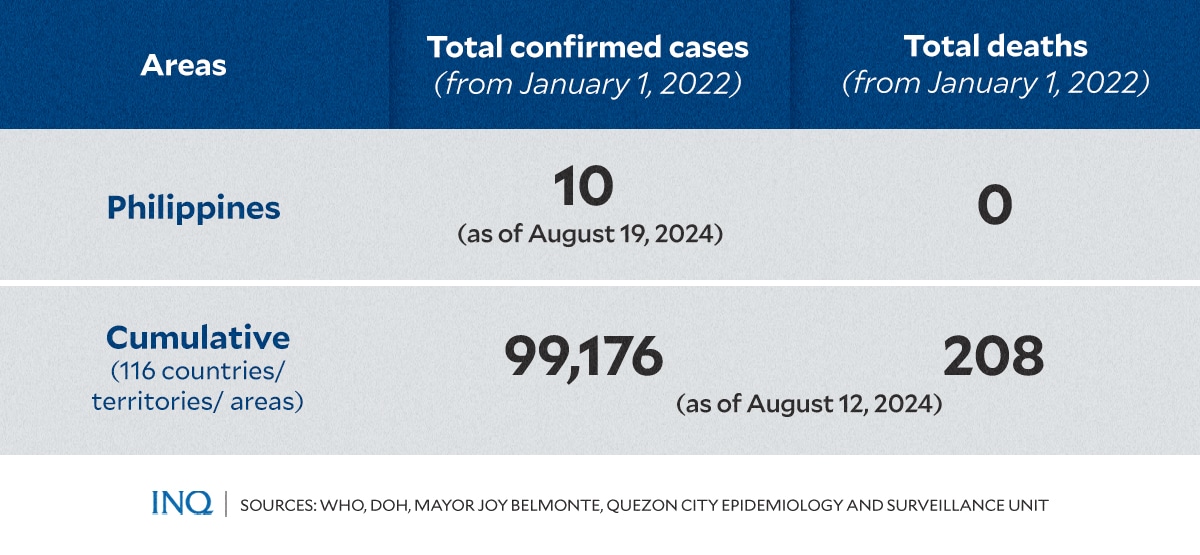
MANILA, Philippines—Earlier this month, the Department of Health (DOH) confirmed the first mpox (formerly known as monkeypox) case in the Philippines, bringing the total laboratory-confirmed cases in the country to 10 since the global outbreak began in 2022.
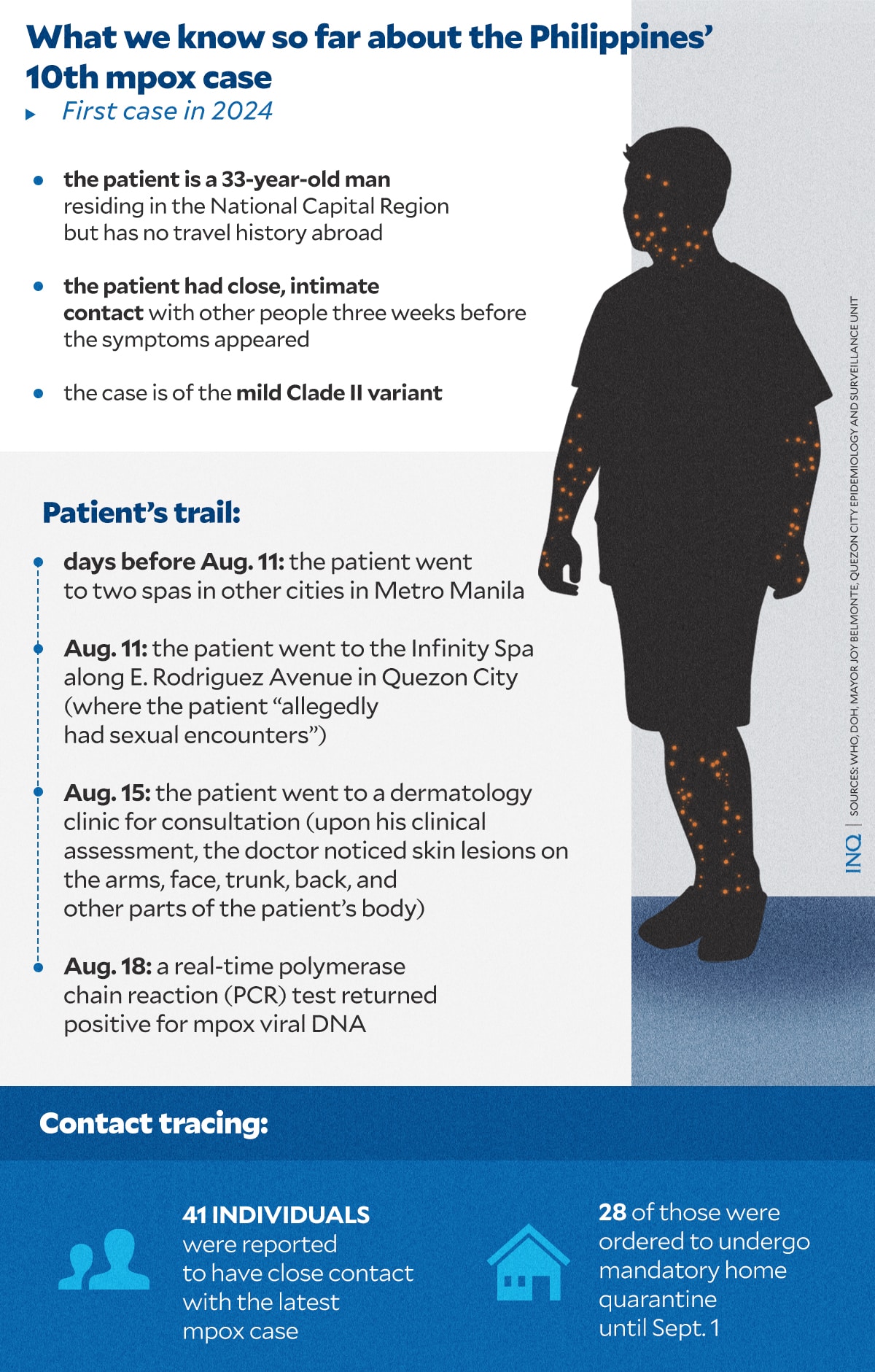
The patient, a 33-year-old male resident of an undisclosed city in the National Capital Region (NCR), tested positive for the virus on August 18, 2024, through a real-time polymerase chain reaction (PCR) test.
The case, which involves the milder variant, highlights the ongoing public health concern surrounding mpox, despite the absence of reported fatalities in the country.
Latest case: What we know so far
According to DOH, the patient has no travel history outside the Philippines but had engaged in close, intimate contact with others weeks before symptoms appeared.
“Symptoms started more than a week ago with fever, which was followed four days later by findings of a distinct rash on the face, back, nape, trunk, groin, as well as palms and soles,” DOH said.
Further investigation by the Quezon City Epidemiology and Surveillance Division (QCESD) revealed that the patient, although not a QC resident, had visited a dermatology clinic in the city for consultation, and likewise had contact with a masseur in a spa.
READ: Quezon City contact tracing first mpox patient – Belmonte
In a press conference last Wednesday, Quezon City Mayor Joy Belmonte detailed that on Aug. 11, the patient went to the Infinity Spa along E. Rodriguez Avenue where he “allegedly had sexual encounters.”
Before this, the patient also said he had visited two similar establishments in other cities in Metro Manila.
Four days later, on Aug. 15, the patient visited a dermatology clinic for a consultation. During the clinical assessment, the doctor observed skin lesions on the patient’s arms, face, trunk, back, and other parts of the body.
The doctor promptly coordinated with the local barangay to arrange the patient’s transport to the Research Institute for Tropical Medicine for specimen collection. On Aug.18, a real-time PCR test confirmed the presence of mpox viral DNA.
In an interview with GMA Super Radyo dzBB on Sunday, Health Secretary Teodoro Herbosa confirmed that the patient has already been discharged and sent home.
What is mpox?
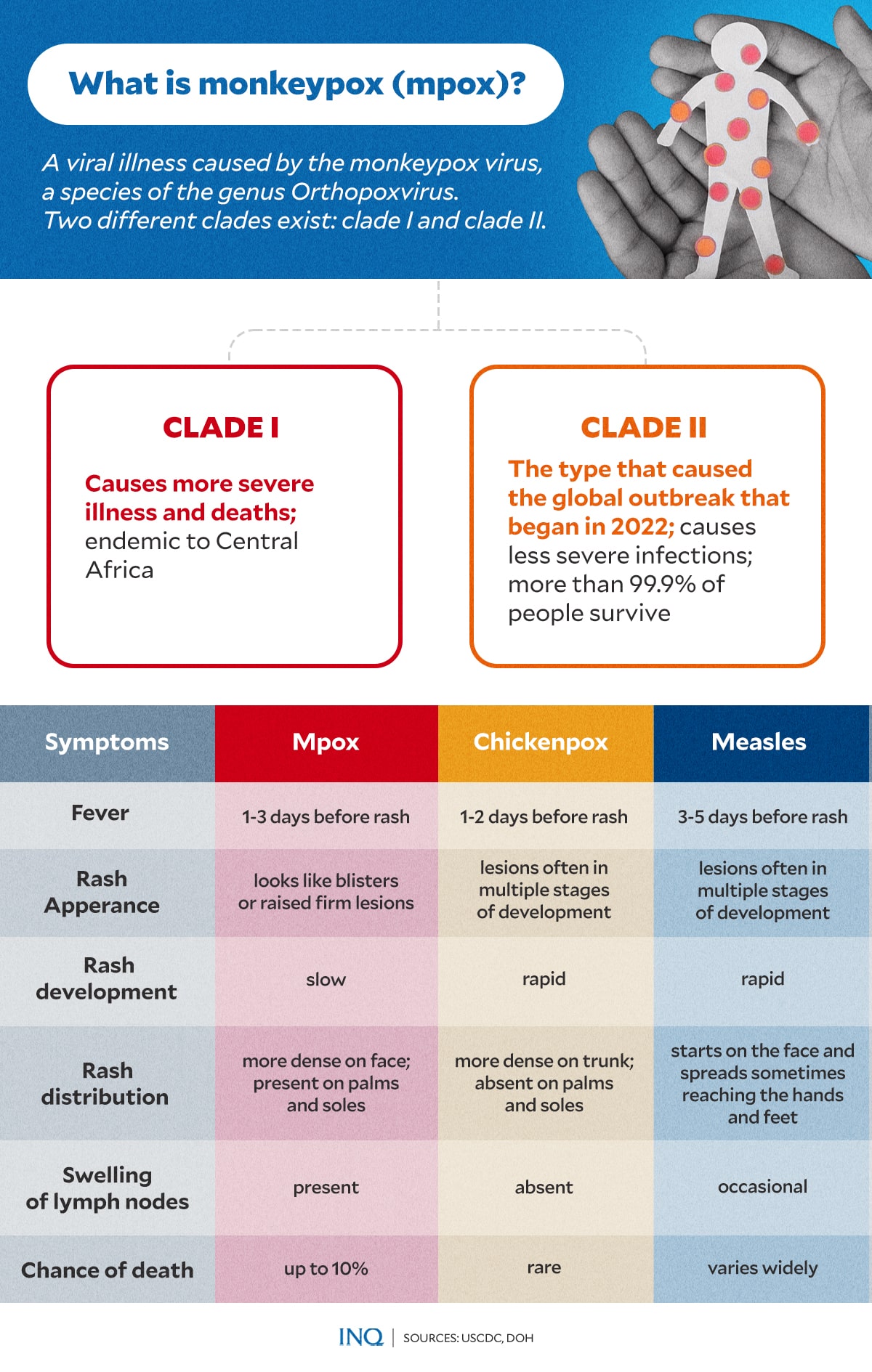
According to the World Health Organization (WHO), mpox is a viral illness caused by the monkeypox virus, which belongs to the Orthopoxvirus genus.
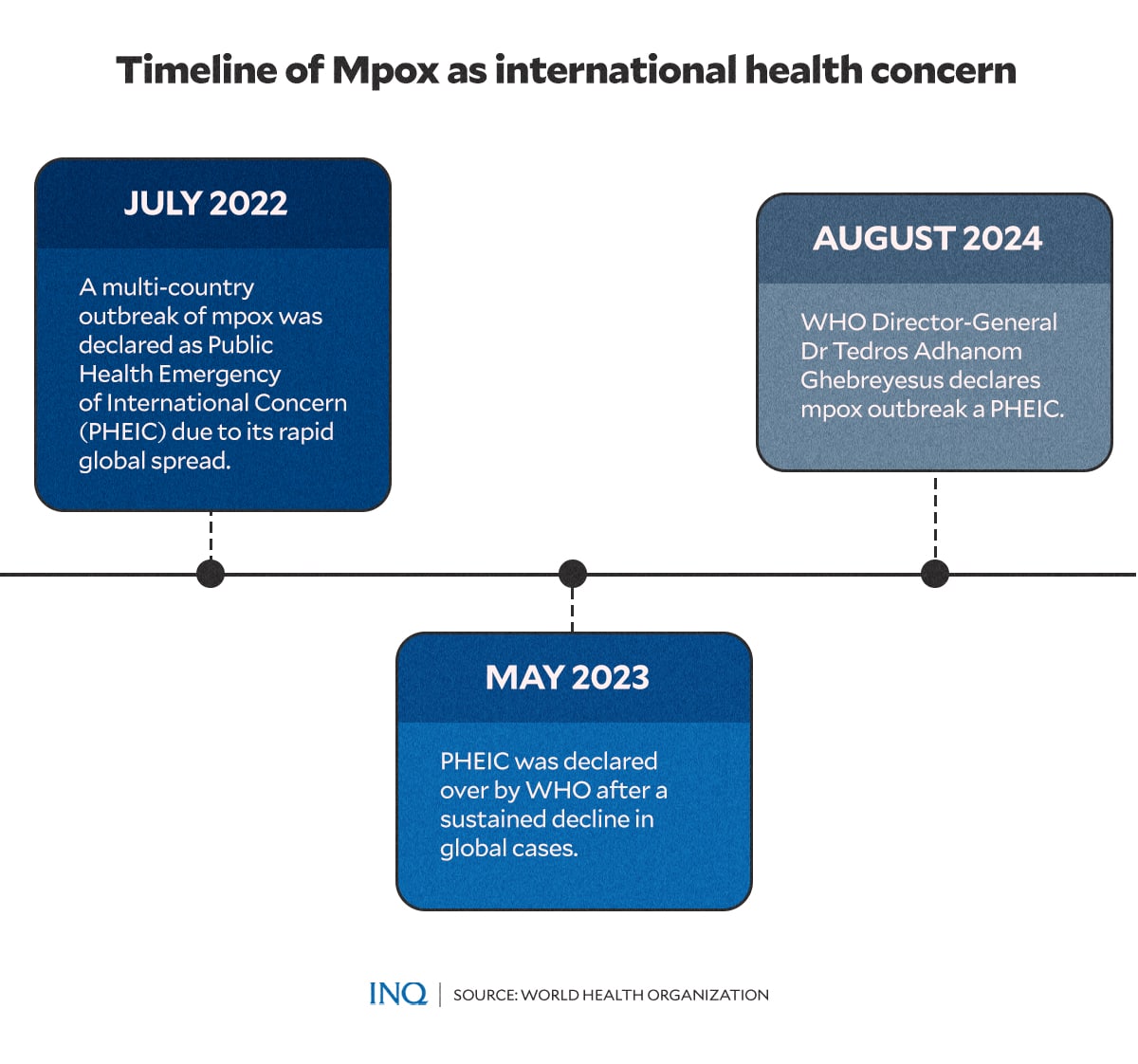
The disease was first identified in the Democratic Republic of the Congo in 1970, but WHO noted that it was largely neglected there. While mpox is endemic in Central and West Africa, it later triggered a global outbreak in 2022.
There are two types of the mpox virus:
- Clade I: This variant is associated with more severe illness and higher mortality rates. The US Centers for Disease Control and Prevention (CDC) reported that some outbreaks of Clade I have resulted in death rates as high as 10 percent, although more recent outbreaks have seen lower fatality rates. Clade I is endemic to Central Africa.
- Clade II: This is the variant responsible for the global outbreak that began in 2022. The CDC noted that infections from Clade II are less severe, with more than 99.9 percent of those infected surviving. Clade II is endemic to West Africa.
The most recent mpox case in the Philippines, along with the nine previously confirmed cases, have all been identified as Clade II.
READ: DOH: Year’s 1st mpox patient contracted the less severe form
How it spreads, what to watch for
Both types of the mpox virus can spread through direct contact with the rashes, scabs, or body fluids of an infected person. It can also spread through prolonged close contact, including sexual contact, and by touching contaminated items like clothing or bedding.
Pregnant individuals can pass the virus to their fetus.
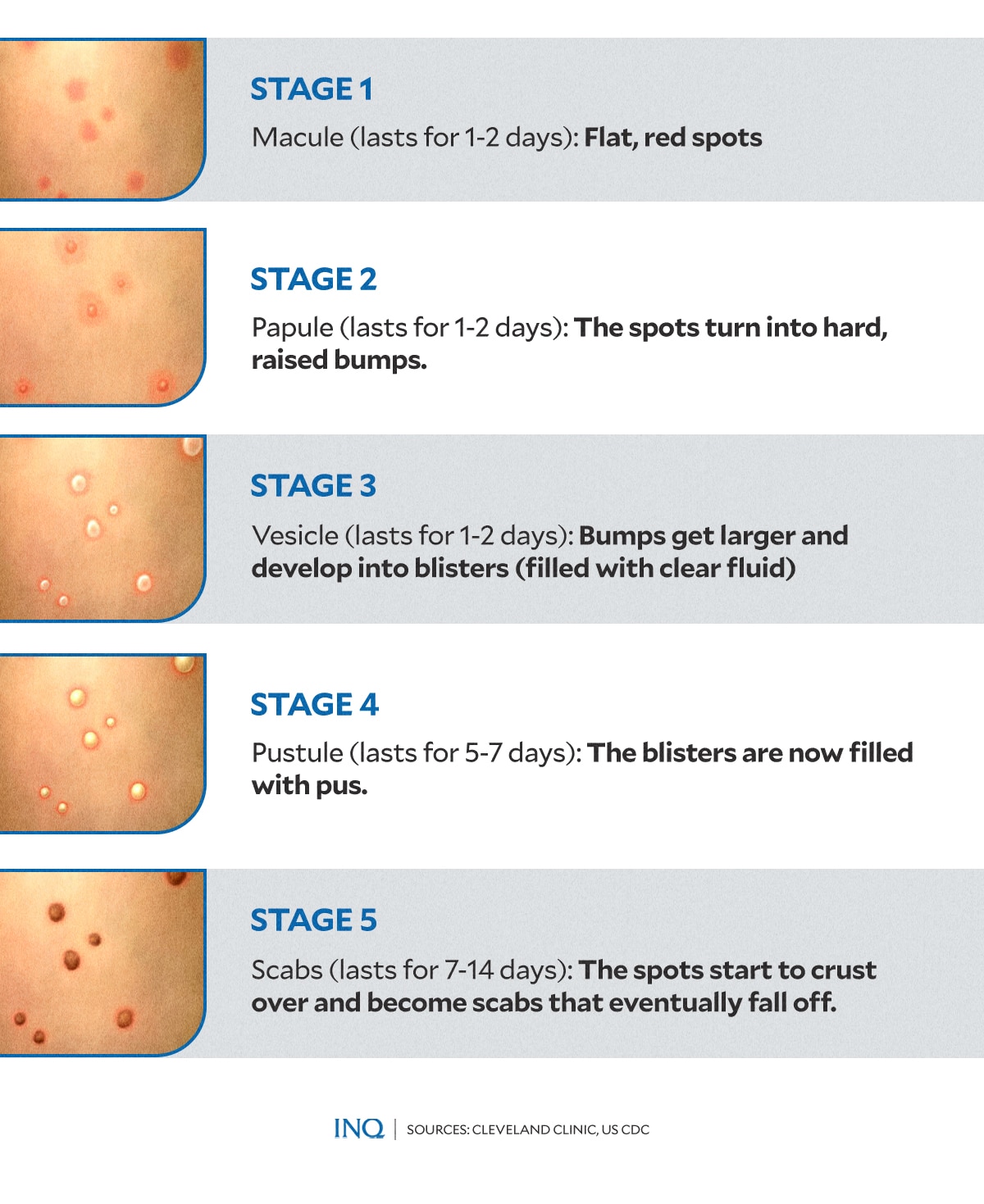
Symptoms usually appear 3 to 17 days after exposure and can last from 2 to 4 weeks. These symptoms include a rash that progresses through five stages — from flat, red spots to raised bumps, blisters, and finally, scabs — as well as fever, swollen lymph nodes, and muscle aches.
READ: Mpox signs and symptoms
The US-based Cleveland Clinic emphasized that not everyone infected with mpox will exhibit all symptoms. However, even with mild or minimal signs, it’s still possible to transmit the virus to others through prolonged close contact.
Among the people who may be more likely to get infected and severely ill include:
- people with severely weakened immune systems
- children younger than 1
- people with a history of eczema
- people who are pregnant
Challenges in contact tracing
Epidemiologist Dr. Rolando Cruz reported that 41 close contacts of the patient have been traced, including his masseur and 27 other patrons of the massage spa from Aug. 11. These individuals have been placed under mandatory home quarantine until Sept. 1, with health authorities conducting daily check-ins.
Other close contacts were advised to quarantine at home and monitor themselves for symptoms. Cruz noted that the dermatologist who treated the patient was not required to isolate, as he was wearing a personal protective equipment (PPE) during the consultation
As of Aug. 20, none of the contacts have shown symptoms, particularly skin lesions. Of the 41 contacts, only seven — three employees and four clients — are Quezon City residents. The DOH-NCR has coordinated with other cities where the patient and contacts reside to implement surveillance measures.
However, on Aug, 22, the Quezon City Epidemiology and Surveillance Unit (CESU) revealed that some of the 28 individuals who may have had direct contact with the patient and are more likely to develop symptoms were inconsistent in reporting their condition.
Cruz stated that they are currently uncertain whether these individuals are adhering to home quarantine, as some have been unresponsive and unwilling to communicate with health authorities.
As of Sunday, Herbosa said contact tracing in the case has already been completed.
How to prevent mpox
The DOH reminds the public to adhere to the following health protocols consistently:
- observe respiratory etiquette (covering mouth when coughing or sneezing)
- ensure good airflow
- wash hands frequently with soap and water or an alcohol-based hand sanitizer
- refrain from contact with individuals who have mpox or who are manifesting mpox infection
People who suspect they have monkeypox should isolate themselves and seek medical advice to prevent spreading the virus to others.
According to the Mayo Clinic, treatment for most people with mpox focuses on relieving symptoms. This may involve managing skin damage from the rash, ensuring adequate hydration to keep stool soft, and providing pain relief.
Currently, there is no specific treatment approved for mpox. However, health care professionals may use certain antiviral drugs originally developed for smallpox, such as tecovirimat (TPOXX) or brincidofovir (Tembexa), to treat the condition.
Vaccine gap
The WHO recommends certain vaccines for use against mpox. These vaccines, developed over many years of research initially for smallpox, are newer and safer. Some have been approved in various countries specifically for mpox.
Vaccination is recommended only for those at risk, such as individuals who have been in close contact with a person infected with mpox or those in high-risk groups. Mass vaccination is not currently advised
Travelers who may be at risk, based on a personalized assessment with their health care provider, might also consider getting vaccinated.
According to WHO, mpox vaccines offer some level of protection against infection and severe illness. However, even after vaccination, it is important to continue taking precautions to avoid contracting or spreading mpox.
Immunity takes several weeks to develop post-vaccination, and some individuals may not fully respond to the vaccine. Nonetheless, for those who contract mpox after vaccination, the vaccine still helps protect against severe disease and hospitalization.
While the DOH has recognized the necessity for the vaccine, there is currently no supply available in the Philippines. Most of the vaccine supply is being allocated to African countries experiencing a surge in pox cases.
READ: WHO: Anti-mpox jabs to go to Africa first
“Right now, the smallpox vaccine is being used in other countries to respond to the outbreak. But since the crisis is in Africa, with thousands of cases there, they are prioritizing vaccine distribution in that region,” said Assistant Health Secretary Albert Domingo in a radio interview.
“However, we are very much interested and have already expressed our intent to the WHO. Once the global strategy shifts and vaccine distribution begins, the Philippines is ready and willing,” he added.
In 2022, at the peak of the global monkeypox outbreak, the DOH announced that the country might receive mpox vaccines by 2023. Dr. Maria Rosario Vergeire, then the officer-in-charge of the DOH, explained that the DOH is coordinating with the private sector, which has shown interest in helping procure vaccines for this rare disease.
READ: DOH says the earliest that PH may acquire monkeypox vaccine is by 2023
Related stories:
Health authorities monitor suspected mpox case in N. Samar