New monkeypox data split scientists’ views

INQUIRER FILE PHOTO
MANILA, Philippines—Several deaths have been reported three months since cases of monkeypox were recorded in countries outside West and Central Africa—where the viral infection was common. Recent data, however, have made some scientists see the outbreak from two different points of view.
Monkeypox, a rare disease caused by the monkeypox virus—a member of the orthopoxvirus genus in the family poxviridae—has already been detected in 95 countries that are not endemic (where cases occur naturally) to the monkeypox virus.
Last July 23, World Health Organization (WHO) declared monkeypox a “public health emergency of international concern“ (PHEIC)—the agency’s highest alarm. It indicates that global coordinated response is needed. It could also unlock funding and international efforts to collaborate on sharing vaccines and treatments.
READ: Monkeypox outbreak constitutes global health emergency – WHO
According to data from the US Centers for Disease Control and Prevention (CDC), a total of 59,179 cases of monkeypox have already been recorded globally as of September 13.
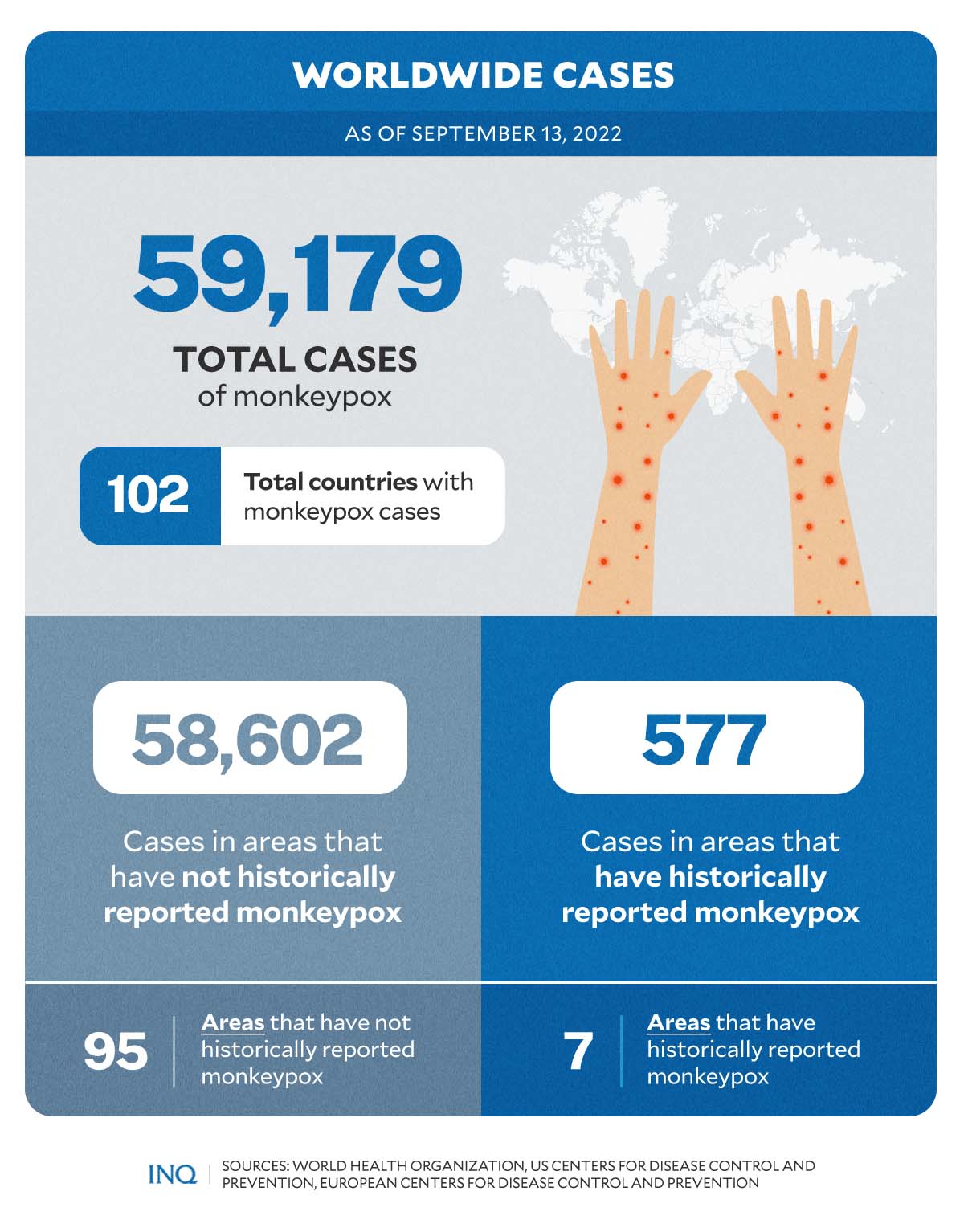
GRAPHIC Ed Lustan
At least 58,602 cases were reported in 95 countries and territories with no historical case of the disease. At least 577 cases were from countries and territories with previous records of the disease even before this year’s global outbreak.
As cases rise, data on monkeypox deaths made some scientists view the current outbreak with a cautious sigh of relief. However, others continued to highlight the severity of monkeypox.
Deaths could be underreported
Based on data collected by the US CDC, there are a total of 19 deaths globally due to monkeypox.
Out of these, 10 were reported in countries that have historically reported monkeypox such as the Central African Republic (2), Ghana (4), and Nigeria (4). The remaining nine deaths were recorded in locations with historically no cases prior to the global outbreak. These include Brazil (2), Spain (2), Cuba (1), Ecuador (1), India (1), and the US (1).
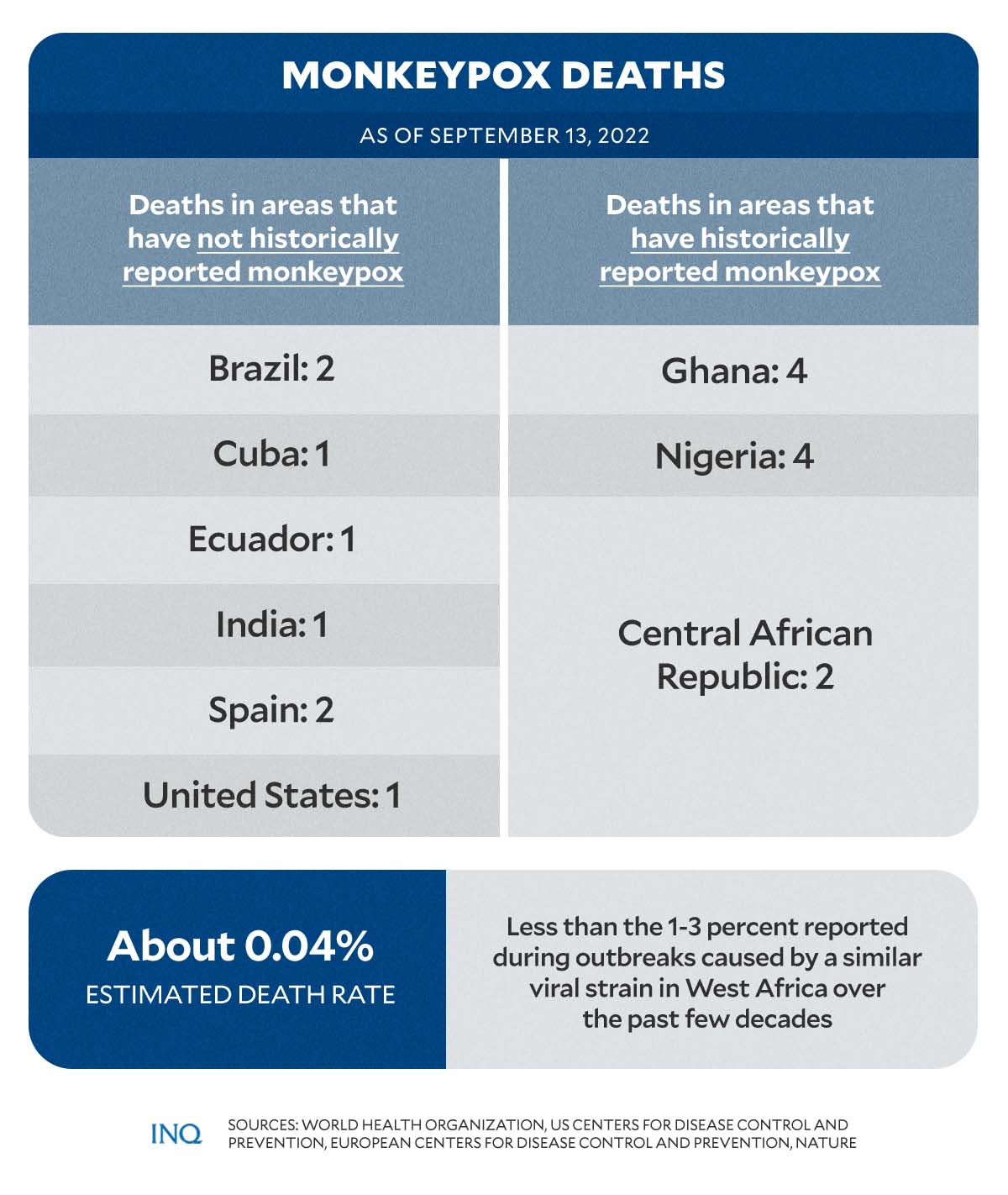
GRAPHIC Ed Lustan
However, according to a recent report published in the peer-reviewed scientific journal Nature, the current death rate—with over 57,000 cases and around 22 deaths—stood at only 0.04 percent.
“That’s significantly less than the 1–3% that has been reported during outbreaks caused by a similar viral strain in West Africa over the past few decades,” the report noted.
“All of this has caused researchers to re-evaluate what they thought they knew about severe monkeypox.”
However, for epidemiologist Andrea McCollum—who heads the poxvirus team at the US CDC—the real number of deaths caused by monkeypox might certainly be higher than the current estimates.
McCollum noted that in places such as Africa, deaths might not be accurately reported and updated due to limited resources for testing and surveillance.
“And it could still rise, especially if the virus spreads more extensively among people at high risk of severe diseases, such as children, older people and those with severely compromised immune systems,” the Nature report stated, citing McCollum.
Severity scale needs fine-tuning
While some scientists heaved a cautious sigh of relief with the recent findings, Jason Zucker, an infectious-disease physician at Columbia University in New York City, emphasized that the disease can be “extremely painful” for those who are infected.
Zucker said monkeypox’s distinctive fluid-filled lesions have been “causing a lot of suffering” among patients. Some people have been hospitalized for life-threatening complications, including difficulty breathing or swelling of the brain.
A detailed case data reported by WHO listed the following as the most common monkeypox symptoms:
- Any rash: 8,587 (90.5%)
- Systemic rash: 6,693 (70.6%)
- Fever: 4,578 (48.3%)
- Genital rash: 3,560 (37.5%)
- Any lymphadenopathy: 2,993 (31.6%)
- Lymphadenopathy: 2,935 (30.9%)
- Fatigue: 2,152 (22.7%)
- Headache: 1,939 (20.4%)
- Muscle ache: 1,738 (18.3%)
- Local lymphadenopathy: 1,615 (17.0%)
- Oral rash: 1,062 (11.2%)
- Asymptomatic: 786 (8.3%)
- Chills: 200 (2.1%)
- Cough: 137 (1.4%)
- Vomiting: 56 (0.6%)
Rashes, according to WHO “evolve sequentially from macules (lesions with a flat base) to papules (slightly raised firm lesions), vesicles (lesions filled with clear fluid), pustules (lesions filled with yellowish fluid), and crusts which dry up and fall off.”
READ: Monkeypox: What to know amid unusual rise in cases
Rashes caused by monkeypox were also found to affect these body parts:
- the face (in 95% of cases)
- palms of the hands and soles of the feet (in 75% of cases)
- oral mucous membranes or the skin inside of the mouth (in 70% of cases)
- genitalia (in 30% of cases)
- conjunctivae or lines inside of the eyelids (in 20% of cases)
According to Zucker, while mucosal lesions are “not inherently more severe,” they aggravate sensitive tissue—which in return can cause intense pain and could interfere with functions such as swallowing, eating, drinking, as well as urinating, and defecating.
Moreover, he noted that mucosal lesions are much harder to identify and characterize compared to skin lesions.
“That means the monkeypox severity scale recommended by the World Health Organization (WHO), which uses number of lesions as a proxy for severity of illness, might need some fine-tuning,” said McCollum.
“This is a reminder that this is not a mild illness. It can be quite serious.”
Monkeypox in PH
Data from the Department of Health (DOH), showed that as of September 14, there are a total of four monkeypox cases in the country.
The first case was reported on July 29, the second and third were confirmed by the health department on August 19, while the latest case was reported on August 22.
READ: First case of monkeypox detected in PH
READ: DOH detects 4th case of monkeypox in PH
The first two cases, according to DOH, were already considered recovered and discharged from isolation.
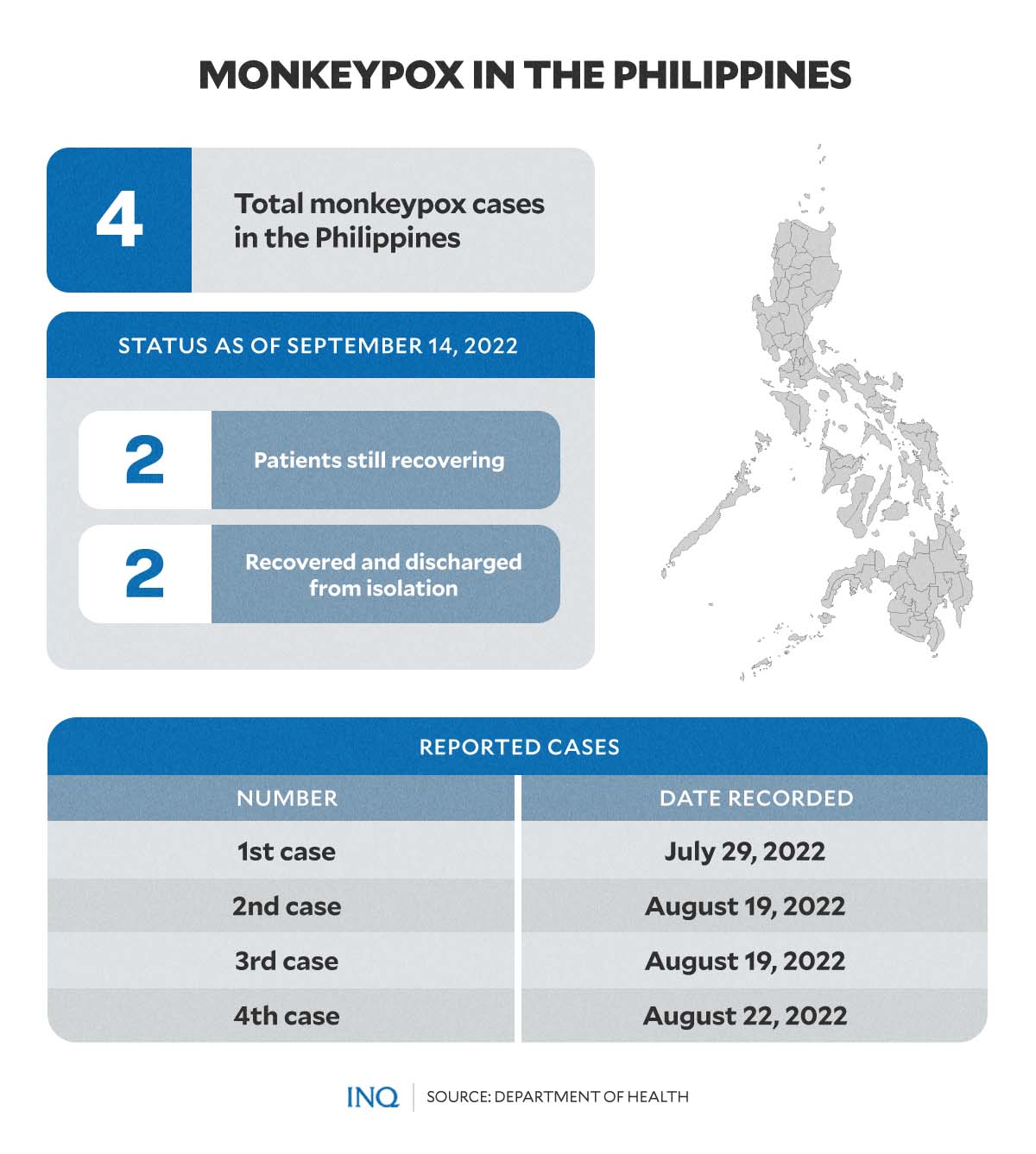
GRAPHIC Ed Lustan
Two other patients are still recovering.
“While the 21st day of [the] case was last August 31, [the] case is not yet declared as recovered since not all of the scabs have fallen off yet,” the DOH said. “Status of lesions has not yet met the required lesion criteria for discharge from isolation.”