Vasculitis nearly turned Ashton Kutcher blind, paralyzed. What is it?
MANILA, Philippines—“You don’t really appreciate it until it’s gone.” Hollywood actor Ashton Kutcher recently said this as he revealed his year-long battle with vasculitis—a condition that almost took his vision, hearing, and mobility.
Kutcher, known for his role in the American TV series “That ‘70s Show” and is now a venture capitalist, has shared his “terrifying journey” about being diagnosed and living with this rare inflammatory disease.
“You don’t really appreciate it until it’s gone, until you go, ‘I don’t know if I’m ever gonna be able to see again. I don’t know if I’m gonna be able to hear again, I don’t know if I’m going to be able to walk again’,” the actor said in an episode of National Geographic’s “Running Wild With Bear Grylls: The Challenge.”
“I’m lucky to be alive,” he added.
READ: Ashton Kutcher recounts vision, hearing loss due to rare vasculitis: ‘Lucky to be alive’
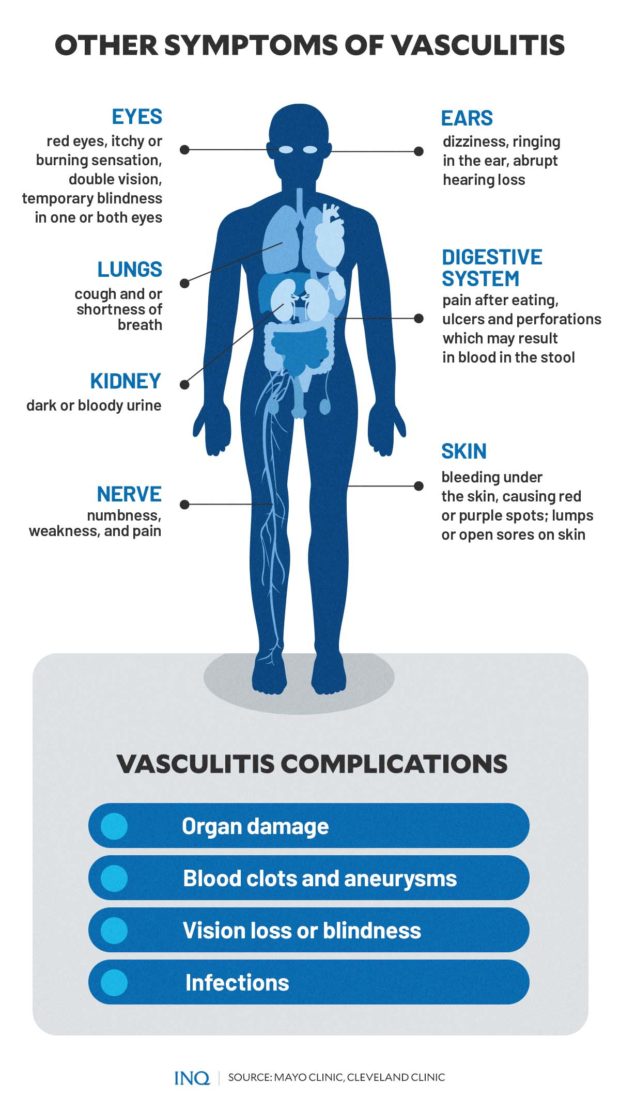
Article continues after this advertisementThis revelation has brought awareness about vasculitis, a little-known autoimmune disease that can affect different parts of the body and lead to complications such as organ damage, blood clots, blindness, and infections.
Article continues after this advertisementUnderstanding vasculitis and its symptoms
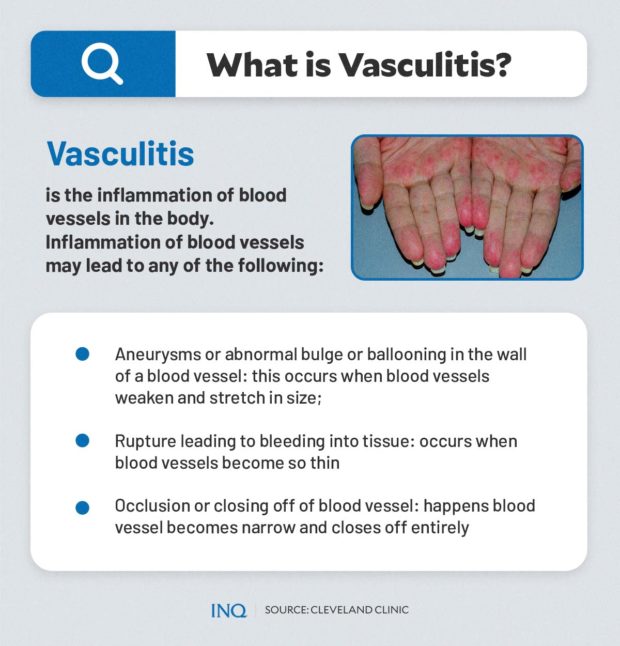
Vasculitis, according to the US National Institutes of Health (NIH), refers to a group of rare medical conditions that occur when inflammation affects the blood vessels in the body.
Inflammation is the immune system’s natural response to an injury or infection. It can lead to swelling, which can help protect the body against invading germs.
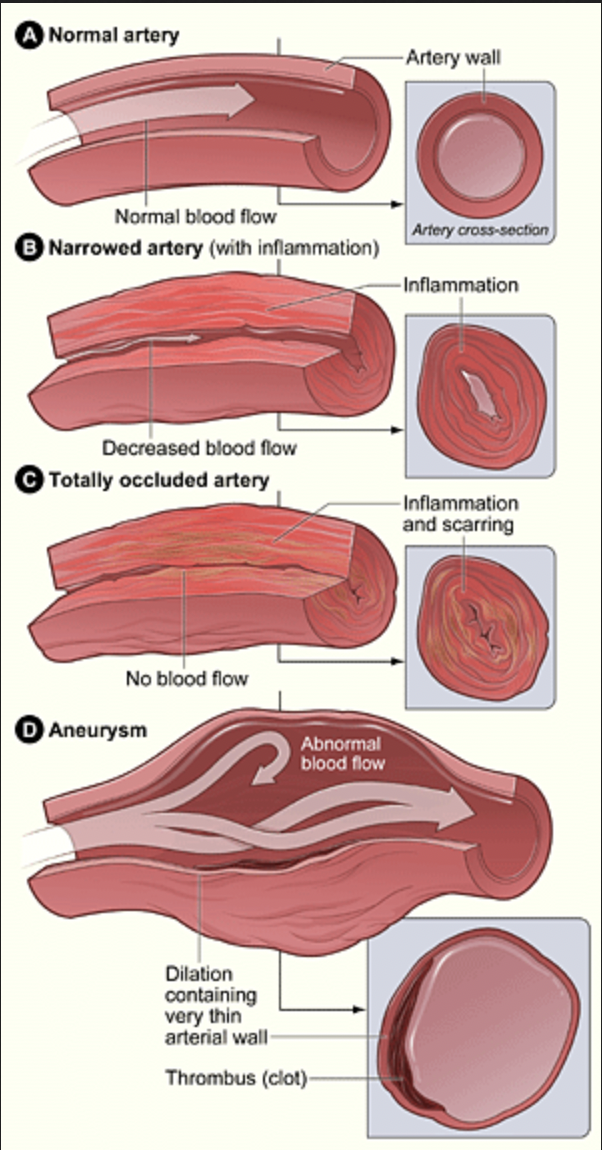
However, in vasculitis, the immune system attacks the healthy blood vessels, making them swollen or narrow.
According to the Cleveland Clinic, inflammation of the blood vessels may lead to any of the following:
- aneurysms or abnormal bulge or ballooning in the wall of a blood vessel—this occurs when inflamed blood vessels weaken and stretch in size
- rupture leading to bleeding into tissue: occurs when inflamed blood vessels become so thin
- occlusion or closing off of blood vessel: happens when an inflamed blood vessel becomes narrow and closes off entirely
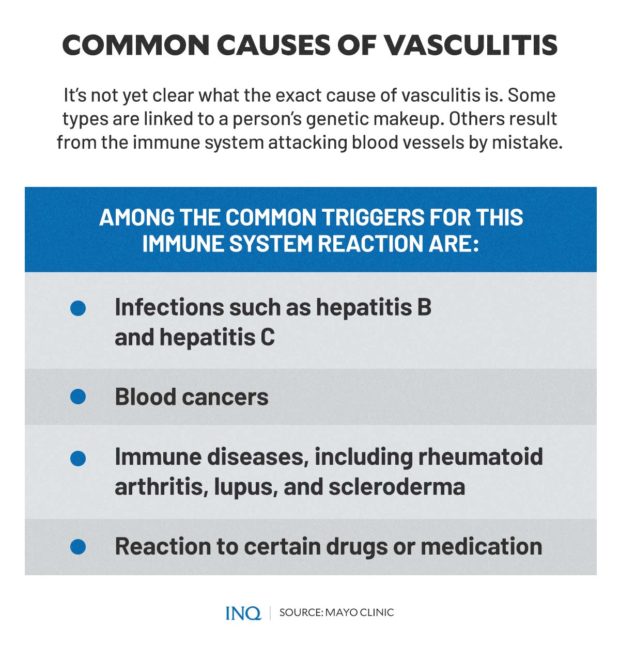
Medical experts have yet to determine the exact cause of vasculitis.
In some cases, the type of vasculitis is influenced by the person’s genetic makeup. Others are due to the immune system attacking blood vessels by mistake.
However, Mayo Clinic said there are common triggers for this immune system reaction, including:
- infections such as hepatitis B and hepatitis C
- blood cancers
- immune diseases, including rheumatoid arthritis, lupus, and scleroderma
- reaction to certain drugs or medication
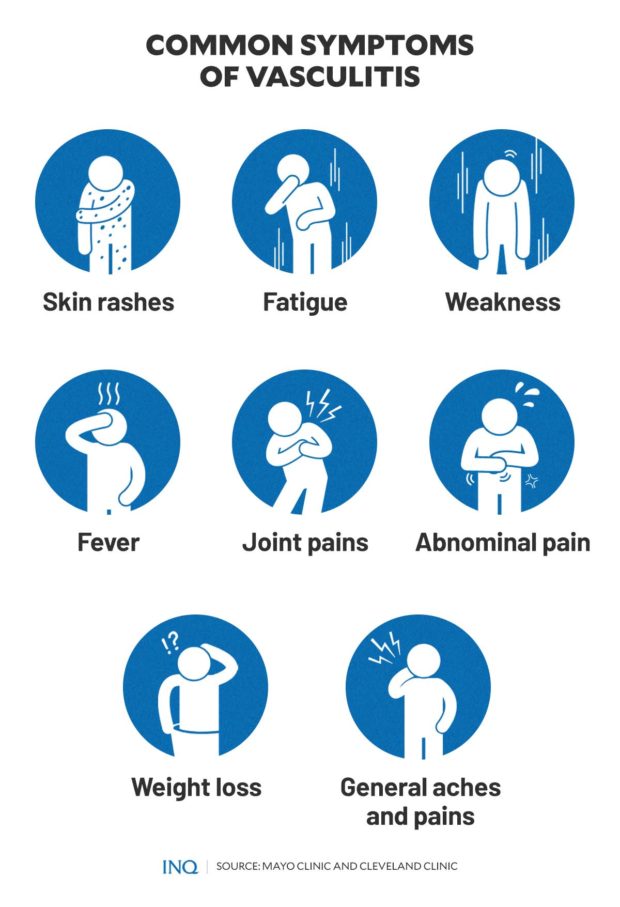
The symptoms of vasculitis also vary depending on the type of vasculitis a patient has, the organs affected, and whether the condition is serious. Some patients also exhibit or experience only a few symptoms, while some become very sick.
“Sometimes the symptoms develop slowly, over months. The symptoms may also develop very quickly, over days or weeks,” the US NIH explained.
Among the general symptoms of vasculitis are:
- skin rashes
- fatigue
- weakness
- fever
- joint pains
- abdominal pain
- weight loss
- general aches and pains
Meanwhile, the following signs and symptoms are related to specific parts of the body affected:
- digestive system: pain after eating, ulcers, and perforations which may result in blood in the stool
- ears: dizziness, ringing in the ear, abrupt hearing loss
- eyes: red eyes, itchy or burning sensation, double vision, temporary blindness in one or both eyes
- kidney: dark or bloody urine
- nerve: numbness, weakness, and pain
- lungs: cough and/or shortness of breath
- skin: bleeding under the skin, causing red or purple spots; lumps or open sores on the skin
Various types and risk factors
There are several types of vasculitis. Some are common, while others are considered rare. Studies also showed that different symptoms appear depending on the type of vasculitis.
Certain types, meanwhile, depend on specific risk factors such as age, family history, lifestyle habits, medications, other medical conditions, race or ethnicity, and gender.
Although vasculitis can happen at any age, there are types that are more common among people of certain ages. These are:
- Buerger’s disease: usually affects men below 45 years old who smoke or have smoked
- IgA vasculitis: diagnosed more often in children than adults
- Giant cell arteritis (temporal arteritis): prevalent among adults aged 50 years old and above and is most common in people who are in their 70s and 80s
- Kawasaki disease: only affects children and is most common among those under the age of 5
These types of vasculitis may run in families:
- Behçet’s disease: typically causes mouth ulcers and genital ulcers; more common in people from Greece, Turkey, the Middle East, China, and Japan
- Granulomatosis with polyangiitis: also known as Wegener’s granulomatosis; affects blood vessels in the nose, sinuses, ears, lungs, and kidneys
- Kawasaki disease
Lifestyle habits, such as smoking and using illegal drugs, were also found to increase the risk of vasculitis.
People with existing medical conditions, like autoimmune disorders, hepatitis B or C, and lymphoma are more likely to be diagnosed with vasculitis.
In June, the “Queen of All Media” Kris Aquino revealed that she was diagnosed with late stage 3 of an extremely rare form of vasculitis: the Churg Strauss Syndrome, also known as Eosinophilic granulomatosis with polyangiitis (EGPA).
According to Aquino’s Houston-based doctor Dr. Niño Gavino, the life expectancy for EGPA without medical intervention is 25 percent, while a five-year survival rate is 62 percent. Only one in one million people are diagnosed with this disease per year.
READ: Kris Aquino diagnosed with rare disease EGPA, says goodbye to fans ‘for now’
Treatment and prevention
Treatment for vasculitis focuses on controlling the inflammation and the underlying conditions that could be triggering the disease.
“The goal of treatment is usually to reduce inflammation,” according to NIH, adding that “people who have mild vasculitis may find relief with over-the-counter pain medicines. For severe vasculitis, you may receive prescription medicine.”
“With treatment, vasculitis can go into remission, which is a period of time when you don’t have symptoms.”
While over-the-counter pain medicines can be enough to relieve symptoms of mild vasculitis, severe cases often require more potent medications prescribed by doctors.
Steroids, such as corticosteroids, are among the common medication given in severe cases. This can help reduce swelling in blood vessels.
In some cases, an attending physician might require procedures or surgery.
In terms of prevention, the NIH noted that some types of vasculitis could not be prevented—primarily if caused by autoimmune disorders.
For some types of vasculitis, medicines may help reduce symptoms. These include:
- anti-clotting medicines to treat blood clots or prevent blood clots from forming;
- beta-blockers which can lower blood pressure;
- statins to control or lower high blood cholesterol levels.
Healthy lifestyle changes—such as adopting a heart-healthy lifestyle, avoiding illegal drugs, and quitting smoking and tobacco—are also recommended to prevent vasculitis.
Vasculitis and COVID-19
In 2020 health experts in New York City and the United Kingdom warned about the possible link between Kawasaki disease, one of the types of vasculitis, and COVID-19 among children ages 2 to 15.
This was after 15 children hospitalized for COVID-19 experienced persistent fever and inflammatory markers similar to Kawasaki disease symptoms. Over half had a rash and experienced abdominal pain, vomiting, or diarrhea. Some had respiratory symptoms.
“We have long suspected that there may be different triggers for KD (Kawasaki disease) based on individual genetics. The emergence of this new problem suggests that the new coronavirus, SARS-CoV-2, may be a trigger for some children to develop KD,” said Jane Burns, director of the Kawasaki Disease Research Center at the University of California at San Diego, in a letter addressed to families of children who have previously had Kawasaki disease.
In the same year, UK’s national health authority issued an alert to warn of an “apparent rise in the number of children of all ages presenting with a multi-system inflammatory state requiring intensive care across London and also in other regions,” which they said could be related to COVID-19.
The US Centers for Disease Control and Prevention (CDC) and some medical experts, however, cautioned against drawing connections between KD and COVID-19.
TSB