Japan OKs world’s first iPS stem cell clinical trial
TOKYO – Japan has given the green light to the world’s first clinical trial using stem cells harvested from a patient’s own body, officials said Thursday, testing a treatment that may offer hope to millions of people robbed of their sight.
A government committee approved proposals for tests aimed at treating age-related macular degeneration (AMD), a common medical condition that causes blindness in older people, using “induced Pluripotent Stem (iPS) cells”, a health ministry official said.
The trial treatment will try to create retinal cells that can be transplanted into the eyes of patients suffering from AMD, replacing the damaged part of the eye.
AMD, a condition that is incurable at present, affects mostly middle-aged and older people and can lead to blindness. It afflicts around 700,000 people in Japan alone.
Stem cell research is a pioneering field that has excited many in the scientific community with the potential they believe it offers.
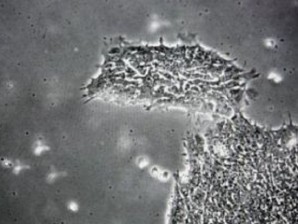
Article continues after this advertisementStem cells are infant cells that can develop into any part of the body.
Article continues after this advertisementUntil the discovery of iPS cells several years ago, the only way to obtain stem cells was to harvest them from human embryos.
This is controversial because it requires the destruction of the embryo, a process to which religious conservatives, among others, object.
Groundbreaking work done in 2006 by Shinya Yamanaka at Kyoto University, a Nobel Laureate in medicine last year, succeeded in generating stem cells from adult skin tissue.
Like embryonic stem cells, iPS cells are also capable of developing into any cell in the body, but crucially their source material is readily available.
Following the government approval, the Riken Center for Developmental Biology will start the world’s first clinical trial using iPS cells as soon as next summer, a Riken spokesman said.
Riken will recruit six patients suffering from AMD, all aged at least 50 years, and take cells from their skin.
These cells will be genetically reprogrammed to become iPS cells. The infant cells will then be nudged in the direction of developing into retina cells.
Once a network of retina cells has been developed — a process that could take around 10 months — this can be transplanted into the patient’s eye, the spokesman said.
Patients will be monitored over the next four years to determine how well the implants have performed, whether the body has accepted them and if they have become cancerous.
“Because no one in the world has used iPS cells in a clinical trial, what we are doing will set the standard,” research leader Masayo Takahashi told the Mainichi, a daily paper. “It’s a daunting prospect, but one that brings joy.”
She said she expects that patients in the initial trial will see only a very modest improvement in their sight.
“We don’t want people to have excessive expectations,” she said.
Kanji Takahashi, chief ophthalmologist at Kansai Medical University Hirokata hospital, told AFP it was a positive step, but not a done deal.
“The trial is a hope for AMD patients, but it will probably take years before the new treatment will actually contribute to improving the vision of many people.”