New stem cell therapy for heart repair shows promising pre-clinical results
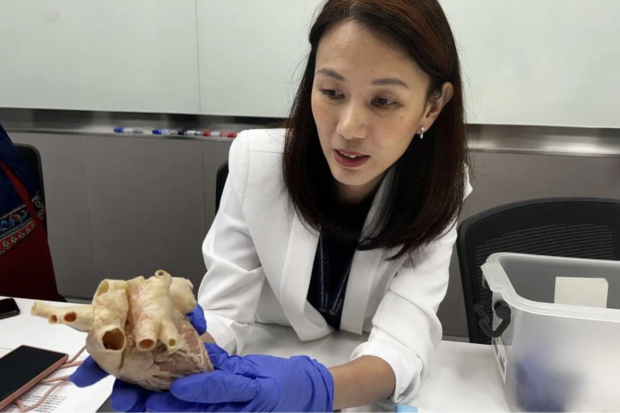
Dr Lynn Yap’s team of researchers at Duke-NUS transplanted immature stem cells into the muscle of the heart damaged by heart attack. The Straits Times/Asia News Network
SINGAPORE – Researchers have long been able to create beating heart cells from stem cells in an attempt to help heart failure patients heal.
But when these cells were implanted into damaged heart muscles in animals, they beat to their own drum and out of sync with the original heartbeat, rendering them discordant and useless for tissue repair.
A new stem cell therapy treatment, developed by a team at Duke-NUS Medical School using immature stem cells, seems to be able to sidestep this problem.
In the study, published in the journal npj Regenerative Medicine in May, immature stem cells were cultivated in the laboratory to grow into heart muscle precursor cells, which can be activated to develop into different types of heart cells.
The most common cause of death worldwide is ischemic heart disease, whereby diminished blood flow to the heart causes the heart muscle cells to die and results in myocardial infarction (MI) or heart attack.
Article continues after this advertisement“The very first course of action for clinics is to open up the vessel using stents to allow blood flow, but there’s already damage. Over time, such patients will develop chronic MI and the heart will slowly fail. When the heart fails, there’s no other treatment for that,” said Dr Lynn Yap, who led the research while an assistant professor at the Duke-NUS Medical School.
Article continues after this advertisementDuring pre-clinical trials, her team injected the immature cells into the area of the heart damaged by heart attack. The cells were able to grow into new heart muscle, restoring damaged tissues and improving heart function. This has shown promising results in pigs.
“This gives us an edge over the beating heart cells. These lesser cells have better potency, and we also saw a reduction in arrhythmia,” said Dr Yap.
In previous studies, the transplantation of heart muscle cells that were already beating brought about fatal side effects such as ventricular arrhythmia – abnormal heartbeats that can limit or stop the heart from supplying blood to the body.
“The current state of the art is using beating cardiomyocytes. So that’s where the problem lies. These actually have their own rhythm. One of these, called the nodal cell, is the pacemaker cell of the heart. So when you transplant something with its own rhythm into an ectopic heart, then there will be two conflicting pacemakers,” said Dr Yap, who is now an assistant professor at the Lee Kong Chian School of Medicine at Nanyang Technological University.
She added that the problem could not be overcome and animals died in many of the pre-clinical studies.
The basis for the immature stem cell project was three decades of work on human proteins called laminin by Professor Karl Tryggvason of Sweden’s Karolinska Institutet and Singapore’s Duke-NUS Medical School.
“Our approach is a new emerging way of treating diseases. The drug is stem cell-derived cells that can replace degenerated tissue or cells and fix the organ or tissue by building new tissues,” said Prof Tryggvason.
“This technology brings us a step closer to offering a new treatment for heart failure patients, who would otherwise live with diseased hearts and have slim chances of recovery.
“It will also have a major impact in the field of regenerative cardiology, by offering a tried-and-tested protocol that can restore damaged heart muscles while reducing the risk of adverse side effects.”
Dr Yap’s team transplanted the immature stem cells into 10 pigs; five of them developed ventricular tachycardia or V-tach, a heart rhythm issue caused by irregular electrical signals in the lower chambers of the heart.
“These five pigs had temporary V-tach that lasted for 30 days but were non-lethal. So we envision that this will happen in half of our patients after they receive the transplant,” said Dr Yap.
“But they would still be in the hospital being monitored. The V-tach can be intervened using drugs to protect them, to keep them safe.”
Dr Yap said the next step for this treatment is to look at controlling the arrhythmia.
“For this current study, I did not use any drug treatment to intervene, so there is room for improvement. Moving forward, I will do a second-generation cell therapy that is safer. We will also be working with a clinician to add arrhythmia-controlling drugs to reduce the incidents. Once this is successful, it will bring us closer towards phase 1 clinical trial,” she said.
Phase 1 clinical trials are usually small trials where a new drug, treatment or medical device is tested in human study participants for the first time.
According to the Singapore Myocardial Infarction Registry Report 2020, there were almost 11,631 heart attack cases that year. This is a rise of almost 60 per cent of the 7,344 cases reported in 2010. The report also said that over 9 per cent of cases died within 30 days.
RELATED STORIES