Cervical cancer: What to know
MANILA, Philippines—This January, the World Health Organization (WHO) underscored the risk of cervical cancer on women’s lives and how vaccines can help protect women across the globe.
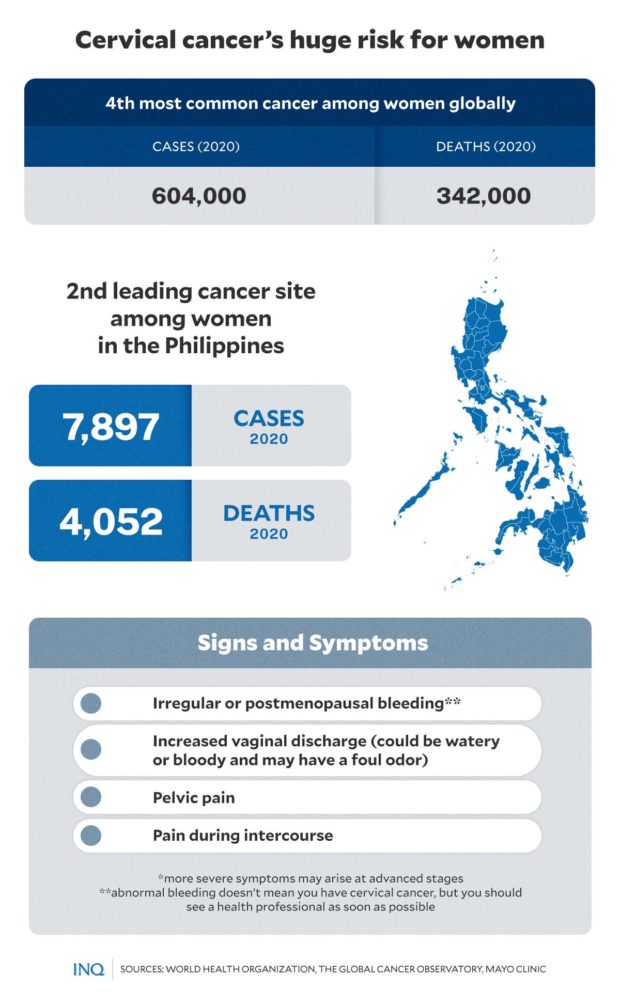
In this year’s cervical cancer awareness month, WHO reminded women across the globe to get informed, screened, and vaccinated against the disease—the fourth most common type of cancer among women worldwide.
The cervix, located at the lower part of the uterus, connects the body of the uterus to the vagina. Cervical cancer, according to WHO, begins when cells lining the cervix start to grow out of control.
Available data showed that in 2020, an estimated 604,000 new cases of cervical cancer and 342,000 deaths were recorded worldwide. At least 90 percent of these cases occurred in low- and middle-income countries.
In the Philippines, data from WHO’s The Global Cancer Observatory detailed that cervical cancer remained the second leading cancer type among Filipino women. In 2020, it was the sixth most common type of cancer overall in the country.
There were 7,897 new cases of cervical cancer recorded in the country that same year. Unfortunately, around 4,000 women also died from the disease.
According to Clarito Cairo, program manager of the National Integrated Cancer Control Program of the Department of Health (DOH), cervical cancer cases averaged 7,200 nationwide annually. Of that number, at least 3,100 women die of the disease every year.
READ: DOH drive aims to curb cases of cervical cancer
HPV and cervical cancer
Nearly all cases of cervical cancers—over 95 percent—are linked to or caused by human papillomavirus (HPV).
“HPV is the most common viral infection of the reproductive tract. Most sexually active women and men will be infected at some point in their lives, and some may be repeatedly infected. More than 90% of the infected populations eventually clear the infection,” WHO said.
However, even though most HPV infections clear up on their own and most pre-cancerous lesions resolve spontaneously, women are still at risk of chronic HPV infections. In some cases, pre-cancerous lesions may also progress to invasive cervical cancer.
Studies showed that women living with HIV are six times more likely to develop cervical cancer than women without HIV. While it takes 15 to 20 years for cervical cancer to develop in women with normal immune systems, in those with weakened immune systems—such as women with untreated HIV infection—cervical cancer may develop in only 5 to 10 years.
HPV vaccination
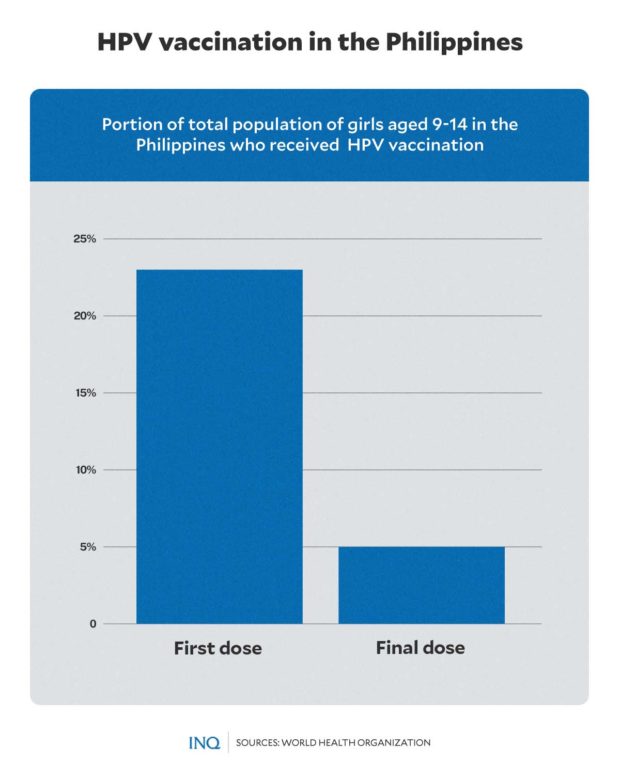
To prevent cervical cancer and reduce cancer risks later in life, the WHO recommends vaccinating girls aged 9 to 14 years with HPV vaccines.
Based on WHO’s cervical cancer country profile for the Philippines, at least 23 percent of girls aged 9-14 years old received their first dose of the vaccine against HPV. Only 1 in 10 girls have received their final HPV vaccination dose.
HPV vaccines are usually given in two or three doses. The social stigma of acquiring sexually transmitted infections (STI) such as HPV, however, has discouraged vaccinees from completing their inoculation, according to Cairo.
In the country, the health department follows the “90-70-90” blueprint for its “Cervical Cancer-Free Philippines” campaign—a 90-percent immunization against HPV for girls 9 to 15 years old; a 70-percent screening for women between 30 and 49; and 90-percent treatment for women testing positive for HPV.
The blueprint represents the global targets set by the WHO’s Global Strategy to Accelerate the Elimination of Cervical Cancer, which every country must reach by 2030.
Acknowledging that vaccination is a cost-effective way to prevent cervical cancer, Cairo said last year that the Health Technology Assessment Council of the DOH has begun reviewing a proposal for a single-dose inoculation against HPV.
“The single dose will definitely be a big help for us,” he said.
READ: One dose of HPV vaccine may prevent cervical cancer
Signs and symptoms
WHO advised women who experience symptoms or suspect they have cervical cancer to be referred to an appropriate facility for further evaluation, diagnosis, and treatment.
Among the symptoms of early-stage cervical cancer may include:
- irregular blood spotting or light bleeding between periods in women of reproductive age
- postmenopausal spotting or bleeding
- bleeding after sexual intercourse
- increased vaginal discharge, sometimes foul smelling.
Meanwhile, severe symptoms may appear as cervical cancer advances. These include:
- persistent back, leg, or pelvic pain
- weight loss, fatigue, loss of appetite
- foul-smell discharge and vaginal discomfort
- swelling of a leg or both lower extremities.
“Other severe symptoms may arise at advanced stages depending on which organs the cancer has spread to,” WHO noted.
Prevention, control, treatment
Aside from HPV vaccination, among the recommended primary prevention for cervical cancer include measures offered to girls and boys, such as:
- health information and warnings about tobacco use
- sex education tailored to age and culture
- condom promotion and provision for those engaged in sexual activity
- male circumcision.
Women aged 30 and above and women living with HIV who are at least 25 years old must follow some preventive measures against cervical cancer, such as
- screening with a high-performance test equivalent or better than HPV test
- immediate treatment or as quickly as possible after an HPV molecular positive test.
Cervical cancer, according to WHO, is one of the most preventable and curable forms of cancer. This type of cancer may be treated through surgery, radiotherapy, chemotherapy, and palliative care.
RELATED STORIES:
11th HPV Summit renews commitment to cervical cancer-free Philippines
It’s #TimeToTalkAboutHPV and chart the path towards a cervical cancer-free Philippines
TSB