Deadly bite: Rabies remains a huge global public health concern
MANILA, Philippines—In the Philippines, March is a significant period for some fur parents—as well as non-fur parents—as it has been marked as rabies awareness month.
Former President Joseph Estrada on March 13, 1999, signed Executive Order No. 84 declaring the month of March as rabies awareness month.
Rabies is a viral zoonotic disease that can infect the central nervous system, or according to the World Health Organization (WHO), can “cause progressive and fatal inflammation of the brain and spinal cord.”
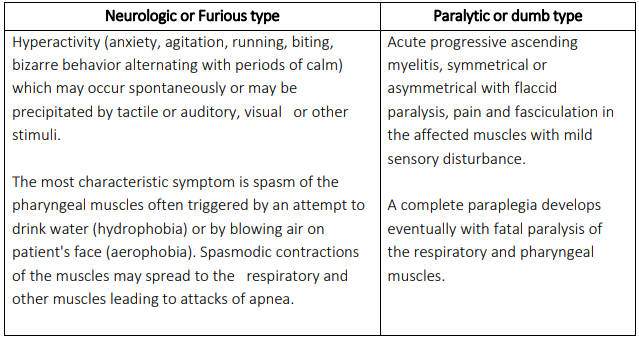
Clinically, rabies has two forms:
- Furious rabies, which the WHO said is characterized by hyperactivity and hallucinations
- Paralytic rabies, which is characterized by paralysis and coma.
According to WHO, the paralytic form of rabies, although accounting for at least 20 percent of the total number of cases across the globe, is often misdiagnosed, contributing to the under-reporting of the disease.
Article continues after this advertisementParalytic rabies also runs a less dramatic and usually longer course than the furious form. Usually, a coma slowly develops, and eventually, death occurs.
In cases of furious rabies, death occurs after a few days due to cardio-respiratory arrest.
The rabies virus is usually transmitted through bites or scratches of an infected animal, usually via saliva.
In this report, INQUIRER.net will detail what you should know about rabies, including preventive measures and treatment methods identified by medical health experts across the world.
By the numbers: Rabies
Data from the Public Library of Science (PLOS) Neglected Tropical Diseases on the Global Burden of Endemic Canine Rabies showed that globally, canine rabies causes at least 59,000 human deaths, over 3.7 million disability-adjusted life years (DALYs), and around P446 billion ($8.6 billion) in global economic losses annually.

Map of countries at risk for rabies around the world. In green: no risk, in yellow: low risk, in orange: medium risk, in red: high risk. MAP BY WHO.
The DALYs is a measure of overall disease burden expressed as the cumulative number of years lost due to ill-health, disability, or death.
The billion-dollar annual economic burden is primarily due to premature death (55 percent), followed by direct cost of post-exposure prophylaxis, or PEP (20 percent) and list of income while seeking PEP (15.5 percent).
In a 2019 report, the Department of Health (DOH), citing data from the WHO, said that as of 2013, 95 percent of rabies deaths occurred in Asia and Africa—“where the presence of three things are common: poverty, poor sanitation, and crowding.”
“The estimated annual figure of almost 60,000 human rabies deaths is probably an underestimate,” DOH said.
Rabies remains to be endemic and a public health concern in the Philippines, according to DOH.
Prior to the COVID-19 pandemic, the health department considered rabies as the most fatal among infectious diseases, with a fatality rate of almost 100 percent.
At least one-third of deaths due to rabies in the country occur in children aged 15 years old and below.
The number of animal bite cases reported in the Philippines increased by 462 percent from 2009—with a total of 206,253 bite cases—to 1,159,711 bite cases recorded in 2018.
The number of positive human rabies cases in the country likewise increased by 13.5 percent from 243 cases reported in 2009 to 276 in 2018.

A historic photograph depicting a Centers for Disease Control (CDC) lab worker, as he was filling a syringe with rabies vaccine that had been obtained from the Alabama State Board of Health located in Montgomery, Alabama. PHOTO FROM US CDC
Still, the US Centers for Disease Control and Prevention (CDC) clarified that it is difficult to estimate the total global burden of rabies by using only human mortality data.
“Rabies is not, in the natural sense, actually a disease of humans. Rather, it is a disease found in wild and domestic animals that can cause cases in humans,” the CDC said.
“Therefore, a more accurate projection of the impact of rabies should include an estimate of the impact on animal populations—particularly domestic animals—and the expense involved in preventing transmission of rabies from animals to humans,” it added.
Animals and rabies
Rabies affects mammals, like raccoons, skunks, bats, and foxes—which accounts for 90 percent of reported cases of rabies that occur in wildlife in the United States. It also affects livestock like cattle and horses.
The virus also affects pet animals like dogs and cats.
In fact, WHO found that 99 percent of rabies deaths across the globe were due to bites of an infected dog.
“[D]og rabies remains common in many countries and exposure to rabid dogs is still the cause of over 90 percent of human exposures to rabies and of 99 percent of human rabies deaths worldwide,” the US CDC stated.
Data by the DOH in 2018 showed that 72 percent of rabies cases were found among canines or dogs that were owned or kept as a pet, while 88 percent of cases were either from free-roaming or occasionally roaming dogs.
It is, however, difficult to determine whether an animal has rabies just by simply looking at it. The US CDC explained that the only way to accurately determine if an animal has rabies is through laboratory tests.
Still, there are some visible signs in animals that might be indicative of rabies.
Some animals with rabies may act strangely or become aggressive, start drooling more than normal, and might try to bite humans or other animals.
Other signs or symptoms to look for in animals include:
- general sickness
- problems swallowing
- excessive drool or saliva
- an animal that is overly aggressive
- an animal that bites at imaginary objects
- an animal that appears tamer than you would expect
- an animal that’s having trouble moving or may even be paralyzed
- a bat that is on the ground
“The signs, symptoms, and outcome of rabies in animals can vary. Symptoms in animals are often similar to those in humans,” said the US CDC.
“These include early nonspecific symptoms, acute neurologic symptoms, and ultimately death,” it added.
Rabies in humans
Infected humans could theoretically transmit rabies through bite and non-bite exposures, but no such case has been documented in the Philippines—nor has it been confirmed globally, according to WHO.
The same applies to transmission to humans via the consumption of raw meat or milk of infected animals.
Most rabies infections among humans are through bites from infected animals like dogs, cats, other domestic animals and wild animals such as bats.
Although rabies from non-bite exposures is less frequent than rabies acquired through bites from infected animals, WHO said it still occurs in some cases.
Some forms of non-bite exposures include:
- Contamination of intact mucosa (eyes, nose, mouth, genitalia) with the saliva of an infected animal
- Licks on broken skin
- Inhalation of aerosolized virus in closed areas (e.g. caves with rabid bats, laboratories for rabies diagnosis)
Following rabies exposure, the rabies virus has to travel to the brain before symptoms occur. This time between exposure and the appearance of symptoms is called the incubation period.
According to DOH, the average incubation period of human rabies can be 1-3 months. In 90-95 percent of cases, the incubation period is less than one year but may be longer in 5-10 percent of cases.
The duration of the incubation period may vary depending on the following factors:
- The amount of the virus inoculated into the wound or mucosa.
- Severity of exposure—Patients with multiple and/or deep penetrating bite wounds may have shorter incubation period.
- Location of exposure—Patients with bite wounds in highly innervated areas and/or close to the central nervous system may have shorter incubation period.
Some symptoms of rabies among humans include:
Furious rabies: hyperactivity, excitable behavior, hydrophobia (fear of water), and sometimes aerophobia (fear of drafts or of fresh air).
Paralytic rabies: muscles gradually become paralyzed, starting at the site of the bite or scratch.
The US CDC noted that the first symptoms of rabies may appear similar to the flu, such as:
- weakness or discomfort
- fever
- headache
- discomfort, prickling, or an itching sensation at the site of the bite
Symptoms can progress to cerebral dysfunction, anxiety, confusion, and agitation and at the same time, the infected person may experience delirium, abnormal behavior, hallucinations, hydrophobia, and insomnia.
“The acute period of disease typically ends after 2 to 10 days. Once clinical signs of rabies appear, the disease is nearly always fatal, and treatment is typically supportive,” said the US CDC.
“Less than 20 cases of human survival from clinical rabies have been documented. Only a few survivors had no history of pre-or post-exposure prophylaxis,” it added.
DOH explained that coma may begin within 4-10 days after symptoms start.
Without intensive support care, respiratory depression, cardiorespiratory arrest, and death occur in almost 100 percent of cases. DOH said 73 percent die within three days of onset of symptoms and 84 percent die within 24 hours of admission.
Cause of death includes circulatory insufficiency with myocarditis, cardiac arrhythmia, or congestive heart failure, according to Research Institute for Tropical Medicine (RITM).
Preventing the fatal disease
To prevent getting infected with rabies, the US CDC urged the public to follow these preventive measures:
- Leave all wildlife alone.
- Understand the risk of contact with both wildlife and domestic animals—especially while traveling internationally.
- Wash animal bites or scratches immediately with soap and water.
- If bitten, scratched, or unsure, talk with a health care provider and ask whether post-exposure prophylaxis (PEP) is needed.
- Remember that rabies in people is 100 percent preventable through prompt appropriate medical care.
- Vaccinate pets to protect them and the people around them.
The US CDC also recommended a set of rabies prevention specifically for pets, which stated that responsible pet owners should:
- Visit veterinarians with their pets on a regular basis and keep rabies vaccinations up-to-date for all cats, dogs, ferrets, and other pet animals.
- Maintain control of pets by keeping them indoors and under direct supervision.
- Spay or neuter their pets to help reduce the number of unwanted pets that may not be properly cared for or vaccinated regularly.
- Call animal control to rescue all stray animals from their neighborhood since these animals may be unvaccinated or ill.
“Rabies is a vaccine-preventable disease. Vaccinating dogs is the most cost-effective strategy for preventing rabies in people,” the WHO said.
“Dog vaccination reduces deaths attributable to dog-mediated rabies and the need for PEP as a part of dog bite patient care,” it added.
Treatment and guidelines
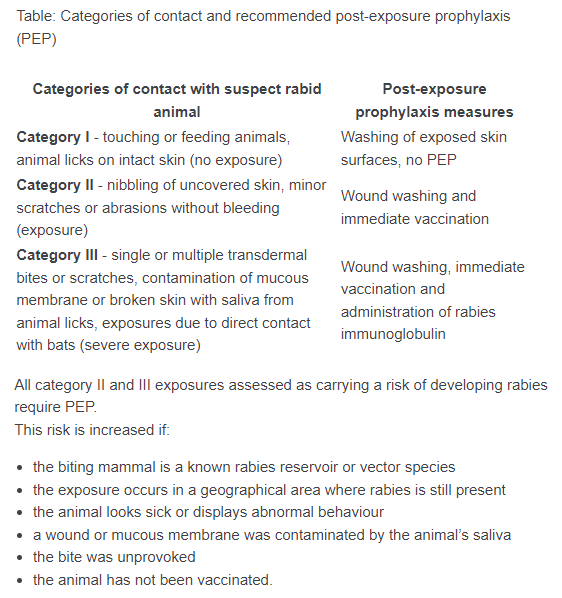
The PEP, according to WHO, is the immediate treatment of a bite victim after rabies exposure. It prevents the virus from entering the central nervous system, which results in imminent death.
The PEP consists of:
- Extensive washing and local treatment of the bite wound or scratch as soon as possible after a suspected exposure
- A course of potent and effective rabies vaccine that meets WHO standards
- The administration of rabies immunoglobulin (RIG), if indicated.
“Starting the treatment soon after an exposure to rabies virus can effectively prevent the onset of symptoms and death,” WHO said.
The administration of the PEP course is recommended depending on the severity of contact with the suspected infected animal.
“The vaccination status of the suspect animal should not be the deciding factor when considering to initiate PEP or not when the vaccination status of the animal is questionable,” said WHO.
“This can be the case if dog vaccination programs are not being sufficiently regulated or followed out of lack of resources or low priority,” it added.