Liver cancer, diseases: A silent epidemic in PH
MANILA, Philippines—During the holiday seasons, many people celebrate by drinking, staying up late, and eating hearty meals—in the Philippines, some staple but heavy dishes included the crispy and fatty lechon or roasted pig.
However, drinking excessive amounts of alcoholic beverages and consuming extra bites of fatty and unhealthy foods during the holidays carry risks to one of the essential organs in our body—the liver.
According to the Department of Health (DOH), the liver has very important functions as it helps break down the food in our stomach, process the nutrients needed by the body, regulate blood clotting, and fight infections due to viruses, bacteria, and other poisonous and harmful sources.
In the Philippines, right after the holiday seasons, the country observe the awareness and prevention month for liver cancer and viral hepatitis
Republic Act No. 10526 signed in 2013 by the late President Benigno Aquino III designated the month of January every year as “Liver Cancer and Viral Hepatitis Awareness and Prevention Month.”
Article continues after this advertisement‘Silent epidemic’
The trend of the still increasing number of Filipinos diagnosed with liver diseases, especially liver cancer, has been described by the National Nutrition Council (NNC) as a “silent epidemic.”
Article continues after this advertisement“Unhealthy lifestyle, largely influenced by Western diet and habits, is said to be among the factors leading to the rising numbers, according to experts,” the NNC said in a statement.
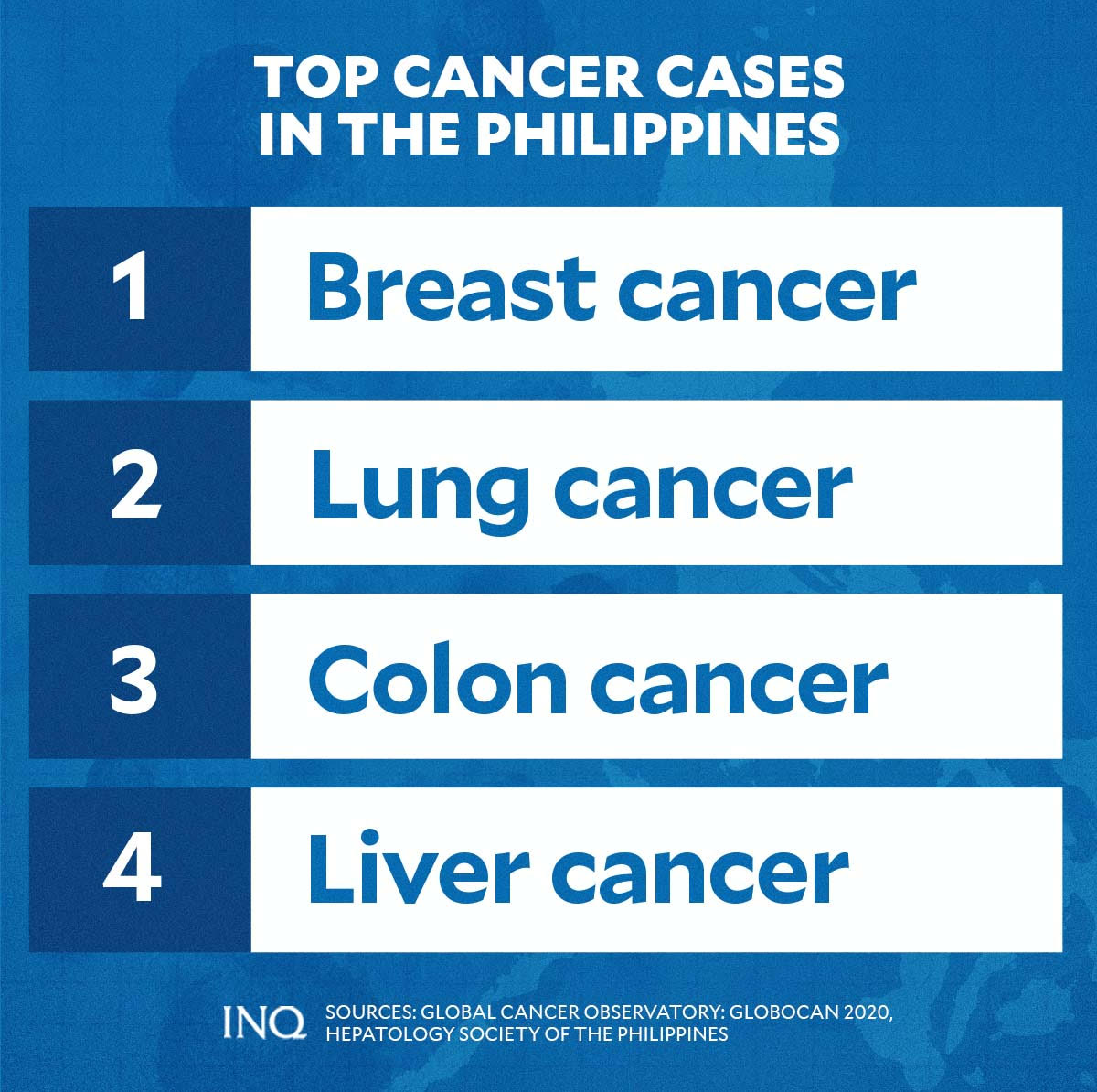
Based on data from The Global Cancer Observatory (GCO) and the Hepatology Society of the Philippines, as of 2020, liver cancer was the fourth most common cancer type in the Philippines after breast cancer, lung cancer, and colon cancer.
During the same year, 10,594 new cases of lung cancer were recorded in the country, bringing the overall number of incidence for both sexes and all ages in the country at 153,751 and a crude rate of 140.3.
The incidence rate of liver cancer among males in the Philippines was 17.8, while it was 6.1 for females.
As explained by the World Cancer Research Fund, this means that men are more likely to have liver cancer than women.
Meanwhile, there were 9,953 new deaths in the Philippines caused by liver cancer in 2020. These figures brought the overall deaths in the country due to the disease to 92,606 and a crude rate of 84.5.
Data from GCO likewise showed that liver cancer’s five-year prevalence was 10,964.
“[The number of lung cancer survivors] is still lower compared to those of breast cancer, colorectal cancers,” Dr. Clarito Cairo Jr., program manager for the cancer control division of DOH, said partly in Filipino.
“This means that we could have more survivors if we can have early detection for liver cancer,” he added.
According to the Makati Medical Center (MMC), there are several types of cancer that can form in the liver, including intrahepatic, cholangiocarcinoma, and hepatoblastoma, and hepatocellular carcinoma—the most common type.
It is more common to see cases of cancer that spread to the liver than cancer that begins in the liver cells.
“Cancer that begins in another area of the body — such as the colon, lung or breast — and then spreads to the liver is called metastatic cancer rather than liver cancer,” Mayo Clinic explained.
“This type of cancer is named after the organ in which it began — such as metastatic colon cancer to describe cancer that begins in the colon and spreads to the liver,” it added.
Signs and symptoms
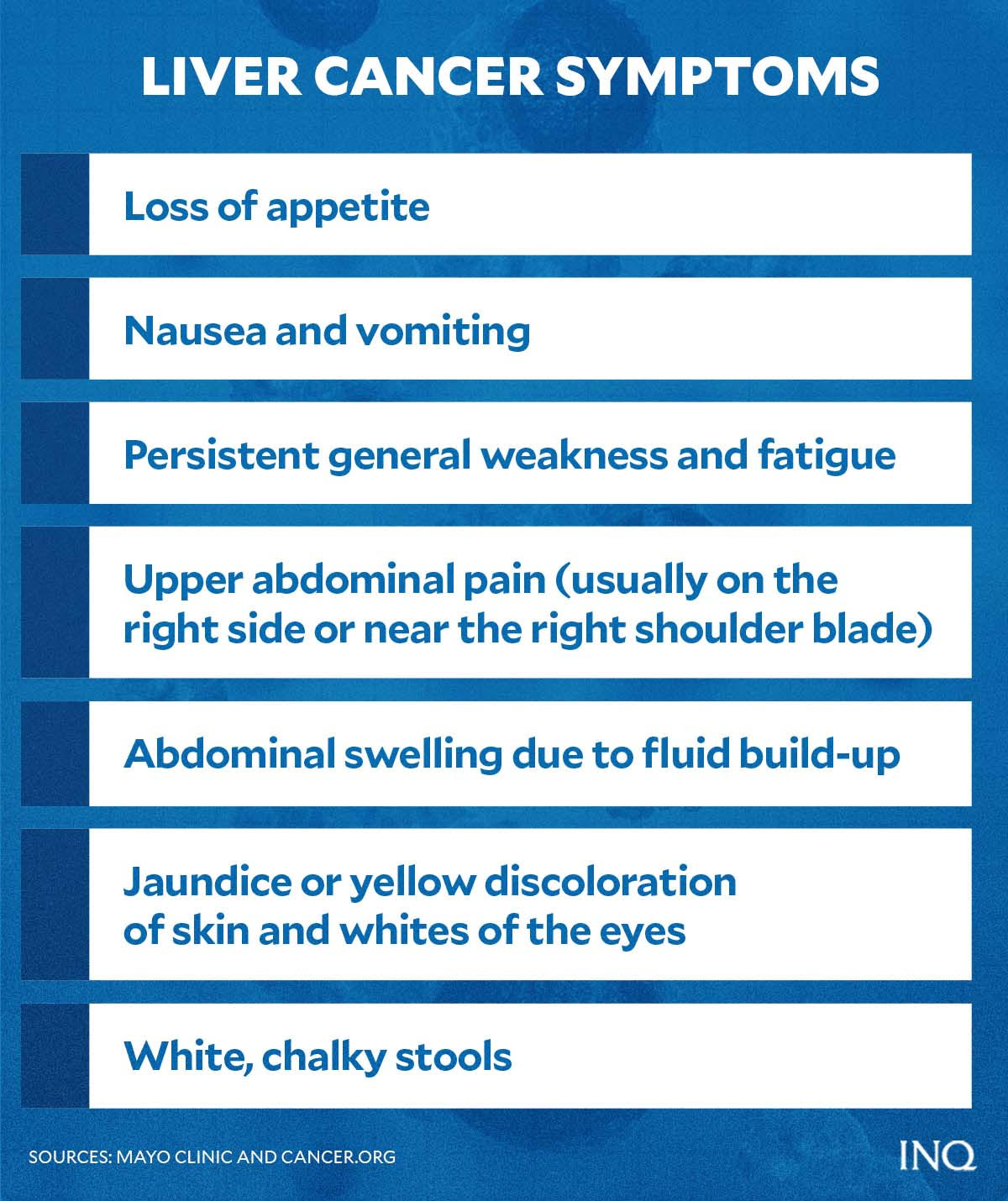
Most people, according to Mayo Clinic, do not experience signs and symptoms in the early stages of primary liver cancer.
Some of the most common symptoms of liver cancer include:
- unintentional weight loss
- loss of appetite due to the malfunction of the liver in the digestive system
- nausea and vomiting
- persistent general weakness and fatigue
- upper abdominal pain (usually on the right side or near the right shoulder blade)
- abdominal swelling due to fluid build-up
- jaundice or yellow discoloration of skin and whites of the eyes
- white, chalky stools
Other symptoms meanwhile include fever, enlarged veins of the belly which can be seen through the skin, and abdominal bruising or bleeding.
The American Cancer Society, however, advised that experiencing one or more of the symptoms does not mean that a person has liver cancer.
Still, the group emphasized the importance of getting checked by a doctor or specialist if any of the symptoms are observed so that the cause can be found and treated if needed.
“Signs and symptoms of liver cancer often do not show up until the later stages of the disease, but sometimes they may show up sooner,” the organization said.
“If you go to your doctor when you first notice symptoms, your cancer might be diagnosed earlier, when treatment is most likely to be helpful,” it added.
Hepatitis and other causes
What causes liver cancer?
According to Cairo, viral hepatitis—specifically hepatitis B and C—is the leading cause of liver cancer cases globally.
Data from the Institute for Health Metrics and Evaluation (IHME) and International Agency for Research on Cancer (IARC) revealed that in 2019, 53 percent of liver cancer deaths were caused by hepatitis B.
At least 26 percent of deaths were caused by hepatitis C.
Deaths due to liver cirrhosis and other chronic liver diseases during the same year were caused by hepatitis B (27 percent), and hepatitis C (30 percent).
Hepatitis, said the World Health Organization (WHO), is a “silent killer” caused by a virus that has no symptoms and “quietly damages the liver for decades before ending in liver cancer and cirrhosis (scarring of the liver that reduces its ability to detoxify blood).”
Dr. Gundo Aurel Weiler, WHO Western Pacific director, said hepatitis B and C cause about 60 percent of liver cancer.
“Studies point to a causal relationship between Hepatitis B virus carrier state and liver cancer. Primary Liver Cancer is much more common in countries where HBV carriers are prevalent, such as the Philippines and other Southeast Asian countries, as compared to most developed countries where Hepatitis B is less prevalent,” said DOH.
“Hepatitis C infection, though less prevalent, can also lead to liver cancer,” it added.
One out of 10 Filipinos is infected with viral hepatitis.
Another common cause of liver cancer, according to the health department is fatty liver.
Fatty liver, DOH said, may also cause liver inflammation and, if not detected and treated early, may lead to liver cirrhosis.
Other causes of liver cancer include:
- genetics
- alcohol abuse
- inherited liver diseases such as hemochromatosis and Wilson’s disease
- non-alcoholic fatty liver disease
- exposure to aflatoxins (poisons produced by molds which can grow on crops that are poorly stored)
- obesity
- type 2 diabetes
COVID-19 and liver disease
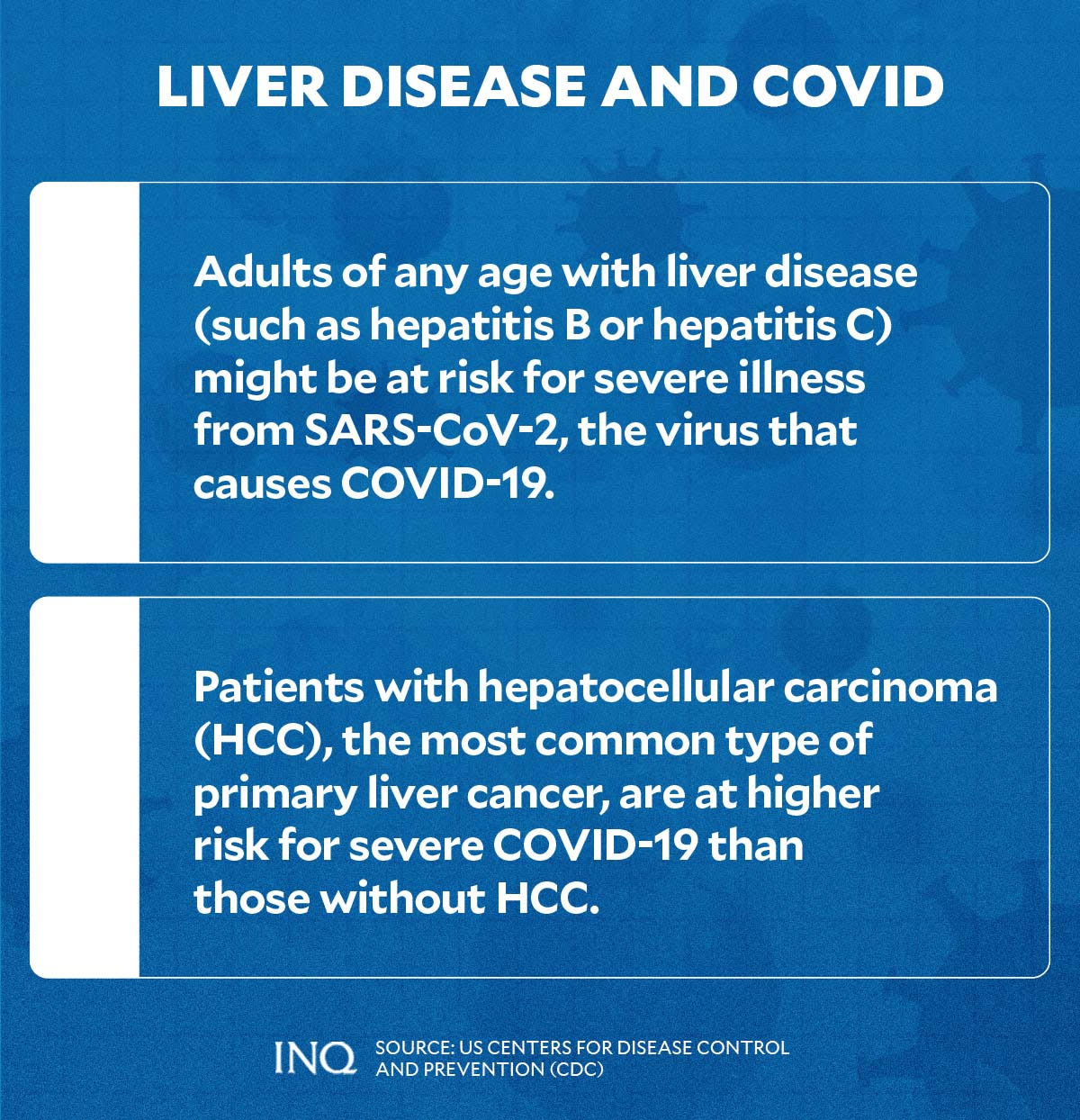
Amid the ongoing pandemic, the United States Centers for Disease Control and Prevention (CDC) noted that adults of any age with liver disease—such as liver cancer, hepatitis B, or hepatitis C—might be at risk for severe illness from SARS-CoV-2, the virus that causes COVID-19.
The CDC added that patients with hepatocellular carcinoma, the most common type of primary liver cancer, are at higher risk for severe COVID-19 than those without HCC.
These were echoed by the Hepatology Society of the Philippines in the recently-released “Clinical Guidance on Liver Involvement in SARS-CoV2 Infection/ COVID-19.”
“Individuals with underlying liver disease may be a vulnerable population, especially those with hepatitis B, liver cirrhosis, and patients on immunosuppression, i.e liver transplant recipients and those with autoimmune hepatitis,” the liver society explained.
“These patients may be at higher risk for SARS-CoV2 infection, may have more severe disease and may have prolonged shedding of the virus causing increased transmission,” it added.
Although COVID-19 primarily affects the respiratory system, the Hepatology Society of the Philippines found liver test derangements in 16 to 53 percent of COVID-19 patients.
They also showed that COVID-19 patients, who are in need of ICU care, are more likely to have a higher percentage and more severe liver test abnormalities due to several factors.
“As the Philippines have a high rate of chronic hepatitis B, it may be prudent to test for the HBsAg status of COVID19 patients, especially when immunosuppression is contemplated as a part of treatment,” the society suggested.
Treatment and prevention
Like for any type of cancer, the DOH said early detection and proper treatment play a huge role in controlling liver cancer.
Blood tests, imaging tests, and removing a sample of liver tissue for testing are some of the tests and procedures which can help diagnose liver cancer.
Some of the available treatments for liver cancer in the country, according to Makati Medical Center, include:
- surgery to remove the affected area in the liver to stop the growth and spread of cancer;
- localized treatment including radiofrequency ablation, cryoablation, alcohol injection, chemoembolization, and radiation;
- targeted drug therapy;
- chemotherapy;
- radiation therapy;
- supprotive (palliative) care;
- liver transplant.
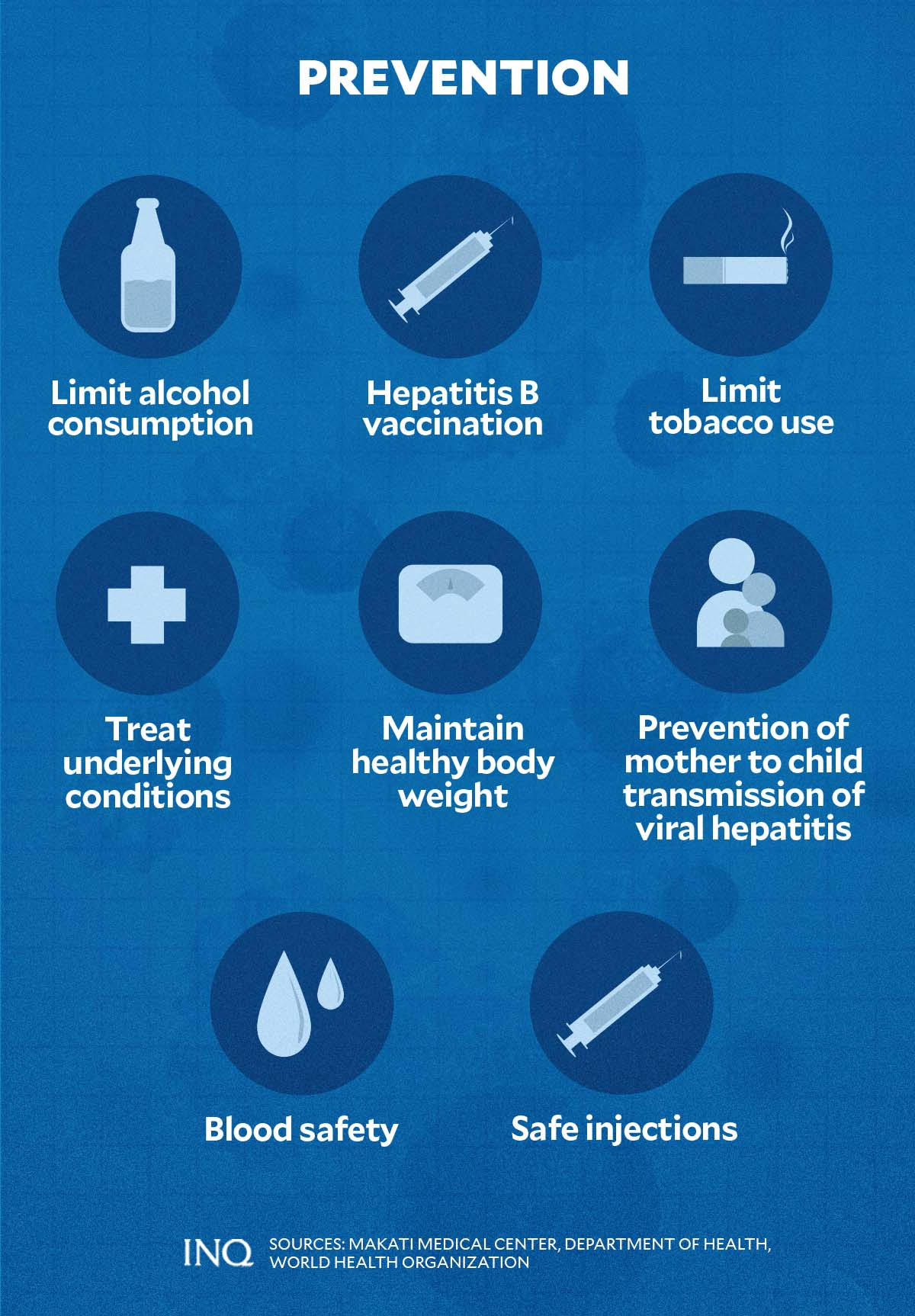
To prevent liver cancer, the health department recommends the following self-care and prevention methods:
- cut back or abstain from alcoholic beverages;
- limit or quit tobacco use;
- maintain healthy body weight through a balanced diet and regular exercise to prevent fatty liver;
- seek treatment for underlying conditions which may cause liver cancer or other complications.
The DOH said individuals are at “greater risk” of exposure to hepatitis B and C when blood, semen, or other bodily fluids from an infected person enter their bodies.
This means that people who use drugs; share needles; are exposed to unsanitary tattoo practices, piercings, or medical equipment; live in prisons and other closed settings; are living with HIV; have unprotected sex with an infected person may get infected with viral hepatitis.
To prevent getting infected, the DOH reminded the public to:
- use sterile, new needles at all times;
- ensure blood safety;
- practice safe sex;
- use safe tattooing and piercing equipment;
- vaccinate infants at birth against hepatitis.
TSB
For more news about the novel coronavirus click here.
What you need to know about Coronavirus.
For more information on COVID-19, call the DOH Hotline: (02) 86517800 local 1149/1150.
The Inquirer Foundation supports our healthcare frontliners and is still accepting cash donations to be deposited at Banco de Oro (BDO) current account #007960018860 or donate through PayMaya using this link.