Low funds, Filipinos’ sexual behavior get in way of HIV cure strides
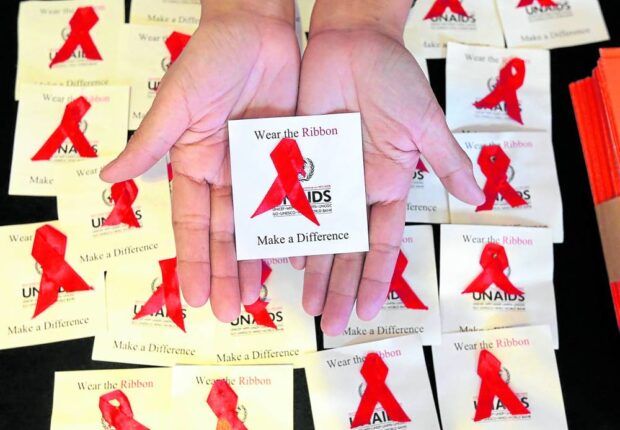
A campaign for awareness on acquired immunodeficiency syndrome (AIDS), the most severe stage of HIV infection. —Marianne Bermudez
MANILA, Philippines — Filipino doctors lauded the progress in the ongoing treatment efforts for the human immunodeficiency virus (HIV). But the Philippines is nowhere near making any breakthrough against HIV because of its scarce funds and poor sexual behavior among the general population, they said.
The recent 25th International AIDS Conference held in late July in Munich discussed several HIV cases that were apparently cured of the virus as well as a new long-acting injectable prevention drug called lenacapavir.
The cost of the drug, however, is prohibitive—at around $42,000 (P2.4 million) per year of treatment.
READ: HIV cases among Filipinos continue to rise, says DOH
But the Guardian, reporting on the Munich conference, cited experts as saying that lenacapavir could be sold for as low as $40 (P2,292.32), which could still reap a 30 percent profit for its manufacturer, US pharmaceutical company Gilead.
Article continues after this advertisementNevertheless, “these scientific breakthroughs are indeed remarkable, incredibly significant progress in responding to HIV,” said Dr. Maria Elena Filio Borromeo, until recently the country director of the Joint United Nations Programme on HIV/AIDS (UNAIDS) in Vietnam.
Article continues after this advertisement“HIV started as having zero treatment with very limited prevention options, mainly on condom use,” said Borromeo, who also headed the STI (sexually transmitted infections)/HIV prevention and control program of the Department of Health (DOH) in the 1990s. But through continued research, she said, HIV could be prevented and treated.
“Now there is increasing evidence of a cure. Such new scientific advancement could significantly improve uninterrupted access to comprehensive prevention, treatment, care and support services,” Borromeo said.
She said if new medicines “will be made universal, funds for lifelong treatment services could be reallocated to prevention and other related services.”
Huge resources needed
But for Dr. Rossana Ditangco, the country faces more pressing priorities, despite the potential promise of new medicines.
“The new medicines are expensive, that’s for sure. But from a public health point of view, will it create a dent if it will be made available in the country?” said Ditangco, who heads the HIV Research Group of the Research Institute for Tropical Medicine, the medical research arm of the DOH.
She said that even if the new medicine might benefit individual Filipinos who could afford it, the government must do the required feasibility studies before purchasing the drug and consider the funds for it.
Dr. Rosario Jessica Tactacan Abrenica, head of the HIV ward of San Lazaro Hospital in Manila, said: “If the drug is made available, it will increase the number of options for prevention.” But she also noted the huge resources needed to make it available.
Dr. Rolly Cruz, head of the HIV program and Quezon City’s Epidemiology and Disease Surveillance Unit, agreed with the prevailing reservations about the breakthroughs in HIV treatment. But he also acknowledged that the new medicine “will have a huge impact and opens another form of prevention strategy.”
“The goal in every new available medical technology should be—the [fewer] people go to the clinic, the better,” said Cruz, who attended the Munich conference.
Abrenica cautioned about the long process of getting the new drug approved by the Food and Drug Administration. According to Cruz, one such preventive drug, pre-exposure prophylaxis or PrEP, still needs implementing guidelines for healthcare professionals.
Unsafe sex behavior
Besides the need for more state and private investments to fund HIV and STI medicines, the doctors also affirmed DOH findings on risky sexual behaviors among the population.
The DOH said 90 percent of all cases of STIs, with HIV being only one of them, are through sexual intercourse.
Young people aged 15-24 years old make up almost 30 percent of all reported HIV infections from 1984 to 2023, and 98 percent were infected through sexual contact.
In a 2022 survey, the DOH said a majority of youth respondents first had sex at 16 and anal sex at 17, but did not use condoms until they were 19 years old.
The US Centers for Disease Control and Prevention, which opened its Manila office in 2022, said the Philippines has the fastest-growing HIV epidemic in the Western Pacific region, with a 411 percent increase in daily HIV incidence between 2012 and 2023.